A Comprehensive Analysis of Impact of Past Medications on Current Admission in a Tertiary Care Hospital: A Prospective Observational Study
2 Department of Pharmacy Practice, St Pauls College of Pharmacy, Turkayamjal, Hyderabad, India
Received: 18-Aug-2021 Accepted Date: Sep 02, 2021 ; Published: 09-Sep-2021
Citation: Nukala A, Vanga H, Kandukuri K, et al. A Comprehensive Analysis of Impact of Past Medications on Current Admission in a Tertiary Care Hospital: A Prospective Observational Study. J Basic Clin Pharma 2021;12(6):76-81.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Background: Drug-Related Problems (DRPs) account for $76.6 billion in hospital costs, 8.7 million hospital admissions, and 17 million emergency room visits annually. Identification and resolution of DRPs predominantly help to achieve better therapeutic outcomes and improved patient care.
Objective: The study aimed to analyse the impact of past medications on current admission in a tertiary care hospital.
Methods: A hospital-based prospective observational study was conducted over a period of six months from October 2019 to March 2020. The necessary data was collected from in-patient case notes, past treatment charts, interviews with patients or patient caregivers and nursing staff. The collected data were analysed using Microsoft Excel 2010 and DRPs were classified based on Hepler and Strand classification and assessed its severity.
Results: A total of 210 patient case sheets were reviewed during the study period. Out of which 75 patients had DRPs, on average of 1 DRP per patient were identified. The most common DRP was adverse drug reaction 66 (88%), drug without indication 5 (6.6%), and sub-therapeutic dosage 2 (2.6%). The majority level of significance of DRPs was seen to have mild 39 (52%), moderate 30 (40%), and severe 6 (8%) impact.
Conclusion: Our present study focuses that adverse drug reaction is the most commonly occurring DRP faced by the patients as an aftereffect of their past medication usage followed by drug use without indication. DRPs that result in hospital admission though most of them are avoidable with little vigilant effort.
Keywords
Drug related problems, Hospital admission, Past medications, Patient care, Severity
Abbreviations
ADR: Adverse Drug Reaction; BMI: Body Mass Index; DRP: Drug Related Programs; PCNE: Pharmaceutical Care Network Europe
Introduction
Medications play a major role in preventing, curing, and treating diseases. But they often also expose patients to Drug-Related Problems (DRPs). According to Pharmaceutical Care Network Europe (PCNE) classification volume 6.2, a drug-related problem is an event or circumstance involving drug therapy that actually or potentially interferes with desired health outcomes. There are a number of consequences associated with the DRPs which include hospitalization, long-term care admission, emergency department visit, additional physician office visit, additional prescriptions, and substantial costs [1]. According to Hepler and Strand Classification, the DRPs are grouped into 8 classifications such as drug use without indication, druginteraction, adverse drug reactions, drug over dosage, and failure to receive medication, sub-therapeutic dosage, improper drug selection, and untreated indications [2].
An international review reported that, 28% of emergency department visits were due to drug-related problems of which 24% were admitted to the hospital. It has been argued that up to 70% of these occurrences were avoidable [3]. In developed countries, few studies have proven that approximately 5% of hospital admissions were due to drug-related problems [4]. Among those 50% were avoidable and it also increases the cost burden and serious consequences on both health care professionals and the health care system [5,6].
In Australian community settings, approximately 90% of patients used to experience one such problem in each. Hence, in health care setup major concern towards DRPs helps to improve patient’s quality of life and prevent extra financial burden in treatment [7]. Approximately 2.4% to 3.6% drug related hospital admissions were reported in Australia [8].
Internationally many studies were conducted on DRPs. In India, very limited research has been conducted to exemplify the impact of DRPs that result in hospital admission though most of them are avoidable with little vigilant effort [9]. Thus there is a need to conduct a study to assess the influence of past medications on the hospital admissions in the Indian scenario as relevant local data is limited. The purpose and objective of this study are to prospectively assess the frequency, severity, and classification of drug-related problems resulting in hospitalization in a tertiary care hospital.
Drug-related problems definitions
Drug use without indication: The patient is taking a medication for no medically valid indication.
Drug interaction: Defined as when the effect of one drug is altered by the presence of another drug, food, a drink, or some other chemical agents.
Adverse drug reaction: Any noxious, an unintended, or untoward medical occurrence, which occurs at doses used in humans for prophylaxis, diagnosis, or treatment.
Study variables: Based on our study the dependent variable is nonadherence of patients to their AEDs and independent variable is demographic variables (age, sex, educational status, marital status, occupation, place of residence, source of medication), patient characteristics (type and number of prescribed AEDs, duration of treatment with AEDs, seizure free period and co morbid conditions).
Drug overdose: The drug product that was taken more than medically recommended dose, resulting in undesirable toxic effects.
Failure to receive medication: The patient is not willing to or able to take the medication therapy as intended.
Sub-therapeutic dosage: The drug product that was taken is too low to produce desired therapeutic response.
Improper drug selection: The patient has a medical problem but is taking a drug which is not indicated to that condition.
Untreated indication: The patient needs drug therapy but not prescribed for the condition.
Materials and Methods
Study setting
The study was conducted in the in-patients wards of a tertiary care hospital in Hyderabad, which is a 300 bedded tertiary care hospital with various departments like general medicine, surgery, paediatrics, psychiatry, pulmonology, neurology, nephrology, ophthalmology gastroenterology, orthopedics, urology, obstetrics and gynecology, ENT, dermatology and radiology.
Study procedure
All the patients admitted in the hospital with significant past medical and medication histories were included in this study. Exclusion criteria includes all the patients treated on out-patient basis, ambulatory patients attributed to poisoning and substance abuse, emergency patients, day care surgery patients, paediatrics and pregnant women. The sources of data were patients demographic details, past histories, in-patient case notes, initial assessment record, laboratory reports on the day of admission, treatment charts and interviewing patients or patients care takers. Case records of the patients admitted in the wards, meeting the inclusion criteria were considered and studied. Data needed for the study was collected and assessed for impact of medications used by the patients in the past on current chief complaints. If DRP is identified, then necessary information was documented in data collection form. A suitable data collection form was designed to collect, document and analyses the data. The data collection form included the provision for collection of information related to patients demographic details like patients age, gender, weight, height, chief complaints, present diagnosis, past medical history (i.e., past medication with dose, frequency, route of administration), initial assessment parameters like blood pressure, pulse rate, temperature, respiratory rate, SpO2, systemic examinations like cardiovascular system, respiratory system, central nervous system and initial laboratory investigations. All the collected data was entered in Microsoft access 2010 for easy accessibility, retrieval and analysis of the data. The Microsoft access format is enclosed as an appendix. DRPs were assessed and categorized based on Hepler and Strand Classification. Data analysis was done by using Microsoft Excel 2010 in a computer and presented in tabulated forms and figure ligands and further statistical analysis was done.
Study design and study duration
A prospective observational study conducted over a period of six months from October 2019 to March 2020.
Results
During the study period, a total of 210 patients were reviewed, out of which 75 patients were enrolled into the study for analyses.
Demographic characteristics of admitted patients due to DRPs
A total of 75 patients, 44 (58.6%) were male and 31 (41.3%) were female patients. Most of the patients were under the age group of ≥ 60 years followed by 18-59 years of age respectively, 55 (73.3%) and 20 (26.7%). 56 (74.7%) patients have BMI less than 29.9 Kg/m2 and 19 (25.3%) patients have BMI more than 29.9 Kg/m2 were presented in Table 1.
| Demographic characteristics | Category | Frequency(n) | Percentage (%) | Ratio |
|---|---|---|---|---|
| Sex | Male | 44 | 58.7 | 1.5:1 |
| Female | 31 | 41.3 | ||
| Age | Adult (18-59yr) | 20 | 26.7 | 01:03 |
| Geriatric ( ≥ 60yr) | 55 | 73.3 | ||
| BMI | >29.9Kg/m2 | 19 | 25.3 | 01:03 |
| <29.9Kg/m2 | 56 | 74.7 |
Note: BMI: Body Mass Index
Table 1: Demographic characteristics of admitted patients due to DRPs, from October 2019 to March 2020 (N=75).
Clinical data of admitted patients with DRPs
In this study, most of the patients have hypertension 56 (37.8%) as their comorbidity followed by diabetes 42 (28.3%), other diseases 18 (12.16%), hypothyroidism 14 (9.46%) and coronary artery disease 14 (9.46%), dyslipidemia 4 (2.70%) and the patients with 2 comorbidities have most of the DRPs 33 (44%) followed by 1 co-morbidity 22 (29.33%) then 3 co-morbidities 14 (18.6%) and 4 co-morbidities 6 (8%). Majority of the patients were stayed more than 5 days i.e., 52 (69.3%). Medical conditions of a patient and length of hospital stay due to DRPs were explained in Table 2.
| Clinical data | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Comorbid conditions | Hypertension | 56 | 37.8 |
| Diabetes | 42 | 28.3 | |
| Hypothyroidism | 14 | 9.46 | |
| Coronary artery disease | 14 | 9.46 | |
| Dyslipidemia | 4 | 2.7 | |
| Others | 18 | 12.16 | |
| Number of comorbidities | 1 | 22 | 29.33 |
| 2 | 33 | 44 | |
| 3 | 14 | 18.6 | |
| 4 | 6 | 8 | |
| Hospital stay | ≤ 5 | 23 | 30.7 |
| >5 | 52 | 69.3 | |
Table 2: Clinical data of admitted patients with DRPs, length of hospital day from October 2019 to March 2020.
Prevalence of DRPs identified and its severity
In this study, most of the DRPs identified were adverse drug reactions 66 (88%) followed by drug use without indication 5 (6.6%), sub therapeutic dose 2 (2.6%), improper drug selection 1 (1.3%) and drug-interaction 1 (1.3%) and the most of DRPs were minor 39 (52%) followed by moderate 30 (40%) and major 6 (8%). Number of DRPs identified and its severity were summarized in Table 3.
| Prevalence | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| DRPs identified | Adverse drug reaction | 66 | 88 |
| Drug use without indication | 5 | 6.6 | |
| Sub therapeutic dose | 2 | 2.6 | |
| Improper drug selection | 1 | 1.3 | |
| Drug interaction | 1 | 1.3 | |
| Severity | Minor | 39 | 52 |
| Moderate | 30 | 40 | |
| Major | 6 | 8 | |
Table 3: Percentages of specific type of DRPs identified and its severity.
Common category of drugs and the type of DRPs developed by each category
In this study, most of the DRPs were developed by anti-hypertensive drugs 35 (31 ADRs, 2 sub therapeutic dosage, 1 improper drug selection, 1 drug interaction) followed by hypoglycemic drugs (10 ADRs), anti-platelets (ADRs), anti-hyperlipidemia drugs (5 ADRs), anti-psychotic drugs 4 (2 ADRs, 2 drug use without indication), antiepileptic drugs (4 ADRs), anti-depressant drugs 3 (1 ADR, 2 drug use without indication), combination drugs (3 ADRs), anti-hypothyroid drugs (2 ADRs ), immunosuppressant drugs (1 ADR) and anti-vertigo drugs (1 drug use without indication) were summarized in Table 4.
| Classification of drugs | Frequency of each DRP | Percentage (%) |
|---|---|---|
| Antihypertensives | ADR(31),Sub-therapeutic dosage (2), Improper drug selection (1), Drug interaction(1) | ADR (41.3%), Sub-therapeutic dosage (2.66%), Improper drug selection (1.33%), Drug interaction (1.33%) |
| Hypoglycemics | ADR(10) | ADR (13.33%) |
| Antihyperlipidemics | ADR(5) | ADR (6.67%) |
| Anti-hypothyroids | ADR(2) | ADR (2.66%) |
| Anti-platelets | ADR(7) | ADR (9.33%) |
| Antipsychotics | ADR(2), Drug use without indication(2) | ADR (2.66%), Drug use without indication (2.66%) |
| Antidepressants | ADR(1), Drug use without indication(2) | ADR (1.33%), Drug use without indication (2.66%) |
| Antiepileptics | ADR(4) | ADR (5.33%) |
| Immunosuppressants | ADR(1) | ADR (1.33%) |
| Antivertigo agents | Drug use without indication(1) | Drug use without indication (1.33%) |
| Combination | ADR(3) | ADR (4.0%) |
| Total | 75 | 100% |
Note: ADR: Adverse Drug Reaction; DRP: Drug Related Problem
Table 4: Frequency of each DRP and the classification of drugs involved.
Category of drugs and their percentage of development of DRPs
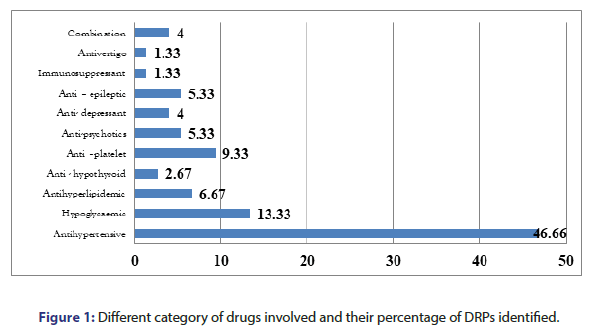
Most of the DRPs occurred in the patients due to anti-hypertensives 35 (46.6%) followed by hypoglycemic agents 10 (13.3%), anti-platelets 7 (9.3%), anti-hyperlipidemia agents 5 (6.67%) and followed by other category drugs usage. Percentage of DRPs identified caused by common categories were summarized in the bar diagram of Figure 1.
Discussion
We conducted a prospective assessment of DRPs related hospital admissions in a tertiary care hospital. We reviewed 210 patients and identified that 75 patients were admitted due to DRPs. In 75 patients, the majority of DRPs occurred in males 44 (58.7%) when compared to females 31 (41.3%). The results are in consistent with earlier study conducted by Wincenty, et al. [10]. Alcoholism, smoking, and a sedentary lifestyle might be the risk factors for the development of more DRPs in males when compared to females. Similar results have been obtained in the earlier study conducted by Mohammed, et al. [11]. There was no gender difference in number of DRPs showed by Zhu, et al. Alexopoulou, et al. and Laribiere, et al. [12-14]. The similar study results were found in Greeshma, et al. and Ramanath, et al. [2,15]. These study findings showed that males were 0.5 times high risk to develop DRPs, which is contrast to the study conducted in, Northwest Ethiopia, Akshaya, Levy, et al. and Roughead, et al. [1,7,16]. The study results were consistent with Abraham and Singh, et al. [9,17]. Females were predominant in DRPs which is contradictory to our study [18]. The current study results were analogous to Abdelaziz, et al. There was no significant difference in gender [19,20].
In our study, geriatrics (age>60 years) are 3 times more risk to develop drug related problems than adults. The mean age of a given population is 63.30 ± 12.98. A similar high rate of hospitalizations due to DRPs in elderly were found in a meta analyses of 17 observational studies which was conducted by Beijer, et al. [21]. In 2018, a study conducted by Greeshma et al. Also found that the incidence of DRPs are more in geriatrics aged (>60 years) than adults age group between (18-60 years) [2]. This might be due to age related changes in pharmacokinetic and pharmacodynamics in elderly patients. This highlights the need of clinical pharmacy services in the patient care unit. Age between 41- 60 years group of people are more prone to develop DRPs, showed in Shareef et al. [22]. Age and DRPs doesn’t have a statistically significant linear correlation [16].
In our study most prevalent disease conditions were hypertension 56 (37.8%) followed by diabetes. The incidence of comorbidities was similar in Greeshma, et al. [2]. An outcome of study led by Patel, et al. 2011 which was conducted in India makes a comparable statistical determination of hypertension and diabetes is the highest [23]. In the current study, among the study population occurrence of DRPs were higher in patients with 2 comorbidities 33 (44%) followed by single comorbidity 22 (29.3%). The results were significantly similar to the study conducted by Greeshma et al. [2]. This was similar to the results obtained by Ahmed, et al. [24]. In the present study, majority of people were hospitalized more than 5 days 52 (69.3%), which was identical to previous reports conducted by Mohammed, et al. and Wincent, et al. [10,11]. The most common DRP in our study population was found to be ADR in 66 (88%) patients followed by drug use without indication 5 (6.6%) patients. In 2016, a study conducted by Ramadaniyati et al, with a similar result of adverse drug reactions is prevalent in-patient populations who are hospitalized [25]. An outcome of ADR is the most commonly occurred DRP in hospitalized patients [2]. Our study results were in contrast with the study conducted by Shareef et al. In which the most commonly occurred drug-related problems were drug interactions [22]. High proportion of ADRs were reported which is analogous our study results [14].
While reviewing the medication chart it was found that 6.6% of drug related problems account for drug use without indication. These study findings are in contrast with the study carried out by Alagiriswami, et al. and Celin, et al. Sub-therapeutic dose was found to be 2.6% in our study [26,27]. This is similar to previous study conducted by Abraham, 2013 [17].
Patients receiving anti-hypertensives are more prone develop DRPs i.e., 46.6% in our current study followed by hypoglycemic and anti-platelets i.e., 13.3% and 9.33%. However, which was less reported DRPs due to anti-hypertensives in earlier study conducted by Greeshma, et al. [2]. Where antimicrobials are more common followed by anti-hypertensives and hypoglycemic. These results were similar with the study published by Komagamine, et al. [28].
In relation to drugs associated with DRPs, our study results i.e., antihypertensives (46.6%), hypoglycemic (13.33%) followed by antiplatelets (9.33%) and anti-hyperlipidemias (6.67%) are most common which was consistent with those of previous studies where drugs were anti-hypertensives, anti-platelets and drugs used to treat electrolyte imbalance [12].
In our results, adverse drug reaction is the common DRP due to antihypertensives. In anti-hypertensives, ARBs (20%) followed by beta blockers (12%), calcium channel blockers (10.6%) and loop diuretics (2.6%). However, which were less similar to results obtained in earlier study conducted by Komagamine et al. It includes diuretics (16%) followed by calcium channel blockers (8%), renin angiotensin inhibitors (6%) and calcium channel blockers (4%) [28].
Of the total 75 DRPs in our study, the level of significance of minor was found to be 52% followed by moderate and severe i.e., 40% and 8%. These study findings are similar to the previous study done by Parthasarathi, et al. [29]. High prevalence of reported DRPs was moderate followed by major in study conducted by Singh, et al. [9].
Conclusion
Most of the DRPs are caused by overlook and/or negligence by the health care workers and are avoidable. The current study indicated that adverse drug reaction is the most commonly occurring drug-related problem faced by the patients as an aftereffect of their past medication usage followed by drug without indication. Males are more prone to develop DRPs than females, Geriatrics are more prone compared to other age groups. The most common category of drugs involved in DRPs was anti-hypertensives, hypoglycemic, anti-platelets, and antihyperlipidemias. Our results highlight the importance and need of wellestablished practices of Pharmacovigilance and the pharmacist linkup with the medical team and the patient to make the patient more vigilant towards their therapy and immediate reporting of adverse effects to the respective authorities. Finally, the pharmacist could help in identifying some drug-related problems by reviewing the past medication chart helps in improving the patient’s quality of life and also reduces the extra financial burden on the patient.
Limitations of the Study
The results of the given study were single centered hence; it may not be generalized to all. Patients with minor DRPs who were visiting the hospital on an outpatient basis are being missed. The study includes less population due to limited time. Our study involved patients who are admitted to medical services of generalization and other services like pregnant women, children, and surgical wards may be limited. Future directions related to our study are warranted to determine in a wide range of populations, establish a strategy that may involve interventions that help to improve prescribing practices and monitoring especially in the patients who are taking high-risk medications or among high-risk patients or patients with multiple comorbidities. Finally, People should be made aware of the incidence, consequences of having medical conditions, and precautions in taking medications by giving proper counseling.
Acknowledgments
Authors would like to thank, Principal, St. Pauls College of Pharmacy, and Head, Department of Pharmacy Practice for their attention, guidance and continues support during the research process.
Ethical approval
The study was conducted after ethical clearance from the Institutional Human Ethical Committee of St. Pauls College of Pharmacy.
Author Contributions
All authors were completely involved in writing proposal, data analyses and interpretation of results; in write up of final research and manuscript preparation and finalization.
Conflict of Interest
There is no conflict of interest.
REFERENCES
- Akshaya SB, Meknonnen BG, Birarra KM, et al. Assessment of drug related problems and its associated factors among medical ward patients in university of Gondar teaching hospital, northwest Ethiopia: A prospective cross sectional. Study J Basic Clin Pharma. 2017; 8:16-21.
- Greeshma M, Lincy S, Maheswari E, et al. Identification of drug related problems by clinical pharmacist in prescriptions with polypharmacy: A prospective interventional study. J Young Pharm. 2018;10:460-465.
- Patel P, Zed PJ. Drug-related visits to the emergency department: How big is the problem? Ann Pharmacother. 2002;22:915-923.
- Einarson TR. Drug-related hospital admissions. Ann Pharmacother. 1993;27:832-840.
- Nelson KM, Talbert RL. Drug related hospital admissions. Ann Pharmacother. 1996;16:701-707.
- Yosef H, Olah-Al, Khalifah M, et al. Admission through the emergency department due to drug-related problems. Ann Saudi Med. 2008;28:426-429.
- Roughead EE, Barratt JD, Sci BA, et al. Medication-related problems commonly occurring in an Australian community setting. Pharmacoepidemiol Drug Saf. 2004;13:83-87.
- Sekhar MS, Mary CA, Anju PG, et al. Study on drug related hospital admissions in a tertiary care hospital in South India. Saudi Pharm J. 2011;19:273-278.
- Singh H, Bithika NK, Sinha T, et al. The incidence and nature of drug related hospital admission: A 6-month observational study in a tertiary care hospital. J Pharmacol Pharmacother. 2011;2:17-20.
- Wincent MM, Potrilingam D, Anagha V, et al. Assessment of drug related problems in patients with chronic diseases in the general medicine units of a tertiary care hospital. Int J Pharm and Pharm Sci. 2017;9:975-1491.
- Mohammed S, Poudel S, Laloo F, et al. Assessment of drug related problems in a tertiary care teaching hospital, India. Asian J Pharm Clin Res. 2017;10:310-313.
- Zhu Y, Liu C, Zhang Y, et al. Identification and resolution of drug-related problems in a tertiary hospital respiratory unit in China. Int J Clin Pharm. 2019;41:1570-1577.
- Alexopoulou A, Dourakis SP, Mantzoukis D, et al. Adverse drug reaction as a cause of hospital admissions: A 6-month experience in a single center in Greece. Eur J Int Med. 2008;19:505-510.
- Laribiere AB, Salame GM, Pochat MC, et al. Incidence of hospital admissions due to adverse drug reactions in France: The EMIR study. Fundam Clin Pharmacol. 2014.
- Ramanath KV, Nedumballi S. Assessment of medication-related problems in geriatric patients of a rural tertiary care hospital. J Young Pharm. 2012;4:273-278.
- Levy M, Lipshitz M, Eliakim M. Hospital admissions due to adverse drug reactions. Am J Med Sci. 1979;277:49-56.
- Abraham RR. Drug related problems and reactive pharmacist interventions for inpatients receiving cardiovascular drugs. Int J Basic Med Sci Pharm. 2013;3:42-48.
- Levy M, Kewitz H, Altwein W, et al. Hospital Admissions due to adverse drug reactions: A comparative study from Jerusalem and Berlin. Eur J Clin Pharmacol.1980;17:25-31.
- Abdelaziz K, Abdelrahim ME. Identification and categorization of drug-related problems on admission to an adult intensive care unit. Eur J Hosp Pharm. 2015;22:138-141.
- Angamo MT, Curtain CM, Chalmers L, et al. Predictors of adverse drug reaction-related hospitalization in Southwest Ethiopia: A prospective cross-sectional study. PLOS ONE. 2017.
- Beijer M, Blaey C. Hospitalisation caused by Adverse Drug Reactions (ADR): A meta-analysis of observational studies. Pharm World Sci. 2002;24:46-54.
- Shareef J, Sandeep B, Shastry CS. Assessment of drug related problems in patients with cardiovascular diseases in a tertiary care teaching hospital. J Pharm Care. 2014;2:70-76.
- Patel V, Chatterji S, Chisholm D, et al. Chronic diseases and injuries in India. Lancet. 2011;377:413-428.
- Ahmed A, Mast MR, Nijpels G, et al. Identification of drug- related problems of elderly patients discharged from hospital. Patient Preference and Adherence. 2014;8:155-165.
- Ramadaniati HU, Anggriani Y, Wowor VM, et al. Drug related problems in chronic kidney disease patients in an Indonesian hospital: Do the problems really matter? Int J Pharm and Pharm Sci. 2016;8:298-302.
- Alagiriswami B, Ramesh M. A Study of clinical pharmacist initiated changes in drug therapy in a teaching hospital. Ind J Pharm Pract. 2009;2:36-45.
- Celin AT, Seuma J, Ramesh A. Assessment of drug related problems in stroke patients admitted to a South Indian tertiary care teaching hospital. Ind J Pharm Pract. 2012;5:28-33.
- Komagamine J, Masaki K. Prevalence if hospitalization caused by adverse drug reactions at an internal medicine ward of a single centre in Japan: A cross sectional study. BMJ. 2019.
- Parthasarathi G, Ramesh M, Hansen KN, et al. Clinical pharmacy in a South Indian teaching hospital. Ann Pharmacother. 2002;36:927-932.