Utilization Study of Antihypertensives in a South Indian Tertiary Care Teaching Hospital and Adherence to Standard Treatment Guidelines
- *Corresponding Author:
- Dr. Supratim Datta
Department of Pharmacology, Sikkim Manipal Institute of Medical Sciences, 5th Mile, Tadong, Gangtok, East Sikkim - 737 102, Sikkim, India.
E-mail: supratimdoc@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Aim: Hypertension represents a major health problem primarily because of its role in contributing to the initiation and progression of major cardiovascular diseases. Concerns pertaining to hypertension and its sequelae can be substantially addressed and consequent burden of disease reduced by early detection and appropriate therapy of elevated blood pressure. This cross‑sectional observational study aims at analyzing the utilization pattern of antihypertensives used for the treatment of hypertension at a tertiary care hospital in perspective of standard treatment guidelines. Materials and Methods: Prescriptions were screened for antihypertensives at the medicine outpatient department of a tertiary care teaching hospital. Medical records of the patients were scrutinized after which 286 prescriptions of patients suffering from hypertension were included. The collected data were sorted and analyzed on the basis of demographic characteristics and comorbidities. Results: The calcium channel blockers were the most frequently used antihypertensive class of drugs (72.3%). Amlodipine (55.6%) was the single most frequently prescribed antihypertensive agent. The utilization of thiazide diuretics was 9%. Adherence to the National List of Essential Medicines (NLEMs) was 65%. The combination therapy was used more frequently (51.5%) than monotherapy (48.8%). The use of angiotensin‑converting enzyme inhibitors/angiotensin 2 receptor blockers (ACE‑I/ARB) was 41.4% in diabetes. Conclusions: The treatment pattern, in general, conformed to standard treatment guidelines. Few areas, however, need to be addressed such as the underutilization of thiazide diuretics, need for more awareness of drugs from the NLEMs and enhanced use of ACE‑I/ARB in diabetic hypertensives.
Keywords
Antihypertensive drug utilization, antihypertensives, pharmacoepidemiology, prescription pattern study
Introduction
Hypertension represents an enormous global public health-care challenge. The World Health Organization (WHO) has projected that 1.5 billion people globally are likely to suffer from hypertension by 2025. [1] The overall prevalence of hypertension in India is estimated at 29%. [2] Cardiovascular diseases are responsible for 1.5 million deaths in India annually. Hypertension is linked to 57% of all stroke deaths and 24% of all coronary event deaths. [3] Hypertension is ranked as the third most important risk factor for attributable disease burden in South Asia. [4] Hypertension is arguably the single most important risk factor for cardiovascular, cerebrovascular, and renal disease that can be modified by timely detection as well as decisive therapeutic intervention.
The guidelines for the treatment of hypertension are put forward by the Joint National Committee (JNC) on detection, evaluation, and treatment of blood pressure. The Indian guidelines, endorsed by the cardiology Society of India, the hypertension Society of India, and the Indian College of Physicians, closely follow the JNC Guidelines (JNC6 and JNC7). [5,6] These guidelines are updated from time to time, based on evidence emanating from basic and clinical research, and guide physicians to select the most appropriate antihypertensive agent in a patient. Pharmacoepidemiological studies such as drug utilization and prescription pattern studies are an important research tool by which the impact that such guidelines have on the selection of therapeutic agents can be assessed and analyzed. It has been observed that evidence-based clinical research is not adequately incorporated into clinical practice, [7] which can in turn result in suboptimal patient health-care practices. The objective of this study is to observe the pattern of utilization of antihypertensives in a tertiary care teaching hospital and relate the findings to current standard treatment guidelines.
Materials and Methods
Data collection
This prospective, cross-sectional observational study was conducted in the Department of Pharmacology and Department of Medicine, Kasturba Medical College and Hospital, Manipal, Karnataka. Before initiation of the study, the approval of the Institutional Ethics Committee was obtained. A predesigned pretested schedule was employed to collect the data. The schedule contained information pertaining to basic demographic variables, comorbid conditions, and a format to assess the antihypertensive drugs prescribed. Patients coming to the medicine outpatient department were screened over a 4-month period. Among all the prescriptions that were screened, prescriptions that had antihypertensive medication as a component were noted along with the hospital number. The corresponding medical files of the patients were accessed from the medical records department to obtain additional information related to the medical history. Hypertensive patients (systolic blood pressure ≥140 mmHg and diastolic blood pressure ≥90 mmHg at the time of diagnosis) were included in the study for the final analysis while nonhypertensive patients and those below 18 years of age were excluded from the study.
Data analysis
Prescribed antihypertensives were classified into five major groups and one miscellaneous group. These included the calcium channel blockers (CCBs) (anatomical-therapeutic-chemical [ATC] classification Code C08), beta blockers (ATC Code C07), angiotensin-converting enzyme inhibitors/angiotensin 2 receptor blockers (ACE-I/ARB) (ATC Code C09), diuretics (ATC Code C03), and alpha blockers (ATC Code C02). Clonidine (ATC Code C02) was included under the miscellaneous group of antihypertensives. Antihypertensive drugs were sorted and categorized on the basis of demographic characteristics (gender and age), number of drugs prescribed (monotherapy and combination therapy), and comorbid conditions (diabetes, ischemic heart disease, and renal parenchymal disease). The National List of Essential Medicines (NLEMs) of India, 2011, Ministry of Health and Family Welfare, Government of India was referred to. Statistical analysis was performed using IBM SPSS statistics version 20 (Statistical Package for the Social Sciences manufactured by IBM Corporation). Chi-square test was applied to analyze the data where appropriate, and P < 0.05 was considered statistically significant.
Results
Demography
A total of 286 hypertensive patients were included in the study. Table 1 gives an overview of the characteristics of the patients and prescriptions. Hypertension was observed to be more common in males (63.6%) than in females (36.4%). The mean age of males was 56.5 ± 15.9 as compared to 53.03 ± 19.3 in females. A total of 68.5% of the patients were in the 18–64 years age range whereas 31.5% were 65 years and above.
| Variable | Value |
|---|---|
| Total number of prescriptions | 286 |
| Total number of antihypertensives prescribed | 511 |
| Gender | |
| Males | 182 (63.6) |
| Females | 104 (36.4) |
| Age (years) | |
| Males (mean±SD) | 56.5±15.9 |
| Females (mean±SD) | 53.03±19.3 |
| 18-64 | 196 (68.5) |
| ≥65 | 90 (31.5) |
| Number of drugs per prescription (mean±SD) | |
| Total | 1.78±0.94 |
| Gender | |
| Males | 1.8±0.97 |
| Females | 1.7±0.89 |
| Age (years) | |
| 18-64 | 1.8±0.06 |
| ≥65 | 1.74±0.1 |
Figures in parenthesis indicate percentage. SD: Standard deviation
Table 1: Characteristics of hypertensive patients and prescriptions
Utilization of antihypertensive drugs
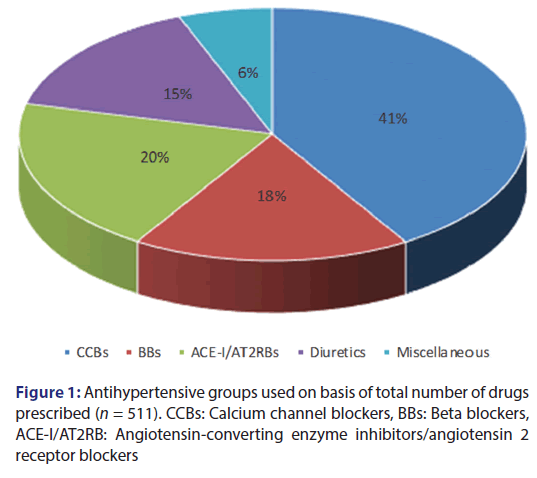
A total of 511 antihypertensive drugs were prescribed during the study (1.78/prescription). Amlodipine was the single most prescribed antihypertensive agent (55.6%), followed by atenolol (17.1%) and enalapril (13.2%). As a class, CCBs were prescribed the most (72.3%) followed by the ACE-I/ARBs (34.9%) and the beta blockers (31.1%) [Table 2]. In terms of total number of antihypertensives prescribed (n = 511), the drug share of CCBs (40.5%) far exceeded that of ACE-I/ARBs (19.6%) and the beta blockers (17.4%). The thiazide diuretics comprised 35% of all the diuretics prescribed and had an overall utilization of 9%. Adherence to the NLEM was the most with the CCBs (98%), followed by the beta blockers (74.4%). Adherence to the NLEM was least with the diuretics (23%). Methyldopa is the only agent from the NLEM that has not been used. Overall adherence to the NLEM was 65%. Figure 1 shows the use of antihypertensive class of drugs on the basis of total number of drugs prescribed (n = 511).
| Antihypertensive drug class | Antihypertensive drug | ATC code | Number of units (n=511) | Percentage use in hypertensive patients (n=286) |
|---|---|---|---|---|
| CCBs | Amlodipine* | C08CA01 | 159 | 55.6 |
| Total=207 (72.3%) | Diltiazem* | C08DB01 | 35 | 12.2 |
| Nifedipine* | C08CA05 | 9 | 3.1 | |
| Felodipine | C08CA02 | 1 | 0.34 | |
| Verapamil | C08DA01 | 3 | 01 | |
| Beta blockers | Atenolol* | C07AB03 | 49 | 17.1 |
| Total=89 (31.1%) | Carvedilol | C07AG02 | 15 | 5.2 |
| Metoprolol* | C07AB02 | 18 | 6.3 | |
| Propranolol | C07AA05 | 2 | 0.7 | |
| Nebivolol | C07AB12 | 5 | 1.7 | |
| ACE-I/ARB | Ramipril | C09AA05 | 38 | 13.2 |
| Total=100 (34.9%) | Enalapril* | C09AA02 | 24 | 8.4 |
| Lisinopril | C09AA03 | 14 | 4.9 | |
| Fosinopril | C09AA09 | 1 | 0.34 | |
| Perindopril | C09AA04 | 1 | 0.34 | |
| Losartan* | C09CA01 | 19 | 6.6 | |
| Telmisartan | C09CA07 | 3 | 1 | |
| Diuretics | Frusemide | C03CA01 | 39 | 13.6 |
| Total=76 (26.5%) | Hydrochlorothiazide* | C03AA03 | 19 | 6.6 |
| Indapamide | C03BA11 | 5 | 1.7 | |
| Chlorthalidone | C03BA04 | 2 | 0.7 | |
| Benzthiazide | N/A | 1 | 0.34 | |
| Spironolactone | C03DA01 | 4 | 1.4 | |
| Amiloride | C03DB01 | 5 | 1.7 | |
| Triamterene | C03DB02 | 1 | 0.34 | |
| Alpha blockers | Prazosin | C02CA01 | 8 | 2.8 |
| Total=9 (3.1%) | Doxazosin | C02CA04 | 1 | 0.34 |
| Miscellaneous | Clonidine* | C02AC01 | 30 | 10.5 |
*Antihypertensive drugs from the National List of Essential Medicines. N/A: Not assigned, CCBs: Calcium channel blockers, ACE-I/ARB: Angiotensin-converting enzyme inhibitors/angiotensin 2 receptor blockers, ATC: Anatomical therapeutic chemical
Table 2: Overall utilization of antihypertensive agents
Utilization of antihypertensive drugs on the basis of gender
Table 3 depicts the utilization pattern of antihypertensive drugs on the basis of gender. The CCBs (χ2 = 0.08, P = 0.77) and ACE-I/ARBs (χ2 = 0.0001, P = 0.99) were prescribed more commonly in males, and beta blockers (χ2 = 0.82, P = 0.36) more in females. Gender-based differences in the use of antihypertensive agents were, however, not significant (P > 0.05 for all groups). Clonidine was prescribed in 3 out of 4 pregnant hypertensive patients.
| Antihypertensive drug class | Males (n=182) | Females (n=104) | P | χ2 |
|---|---|---|---|---|
| CCBs | 138 (75.8) | 69 (66.3) | 0.77 | 0.08 |
| Beta blockers | 55 (30.2) | 34 (32.7) | 0.36 | 0.82 |
| ACE-I/ARB | 66 (36.2) | 34 (32.7) | 0.99 | 0.0001 |
| Diuretics | 50 (27.4) | 26 (25) | 0.97 | 0.001 |
| Alpha blockers | 7 (3.8) | 2 (1.9) | - | - |
| Clonidine | 21 (11.5) | 9 (8.6) | 0.62 | 0.23 |
| Total units | 337 | 174 | - | - |
Figures in parenthesis indicate percentage. CCBs: Calcium channel blockers, ACE-I/ARB: Angiotensin-converting enzyme inhibitors/angiotensin 2 receptor blockers
Table 3: Pattern of antihypertensive drug use on the basis of gender
Utilization of antihypertensive drugs on the basis of age
Table 4 depicts the pattern of antihypertensive drug use on the basis of age. The use of CCBs (χ2 = 0.01, P = 0.9) and beta blockers (χ2 = 2.57, P = 0.1) was more in the age group of 18–64 years than in patients ≥ 65 years. The ACE-I/ARBs (χ2 = 1.62, P = 0.2) and diuretics (χ2 = 5.43, P = 0.01) were used more frequently in patients ≥65 years than in the 18–64 years age group. Significant variation (P < 0.05) in age group-based use of antihypertensives was seen only with the diuretics and clonidine.
| Antihypertensivedrug class | 18-64 years(n=196) | ≥65 years(n=90) | P | χ2 |
|---|---|---|---|---|
| CCBs | 144 (73.4) | 63 (70) | 0.9 | 0.01 |
| Beta blockers | 68 (34.7) | 21 (23.3) | 0.1 | 2.57 |
| ACE-I/ARB | 64 (32.6) | 36 (40) | 0.2 | 1.62 |
| Diuretics | 44 (22.4) | 32 (35.5) | 0.01 | 5.43 |
| Alpha blockers | 5 (2.5) | 4 (4.4) | - | - |
| Clonidine | 29 (14.8) | 1 (1.1) | 0.0008 | 11.23 |
| Total units | 354 | 157 | - | - |
Figures in parenthesis indicate percentage. CCBs: Calcium channel blockers, ACE-I/ARB: Angiotensin-converting enzyme inhibitors/angiotensin 2 receptor blockers
Table 4: Pattern of antihypertensive drug use on the basis of age
Utilization of antihypertensive drugs on the basis of type of therapy
Table 5 depicts the pattern of antihypertensive drug use on the basis of type of therapy. Combination antihypertensive therapy (52.1%) was used more frequently than monotherapy (47.9%). A combination of two antihypertensive drugs has been used the most (59.3%) followed by three drug (31.6%) and ≥4 drug combinations (9%). The use of CCBs (χ2 = 20.96, P < 0.0001), diuretics (χ2 = 18.62, P < 0.0001), and clonidine (χ2 = 4.59, P = 0.03) was more in combination than as monotherapy. Furosemide and the potassium-sparing diuretics have only been used in combination. A total of 28 fixed dose combinations were prescribed of which the most commonly prescribed fixed drug combination was that of amlodipine and atenolol (n = 15).
| Antihypertensive drug class | Monotherapy (n=137) | Combination therapy (n=149) | P | χ2 |
|---|---|---|---|---|
| CCBs | 78 (56.9) | 129 (86.5) | <0.0001 | 20.96 |
| Beta blockers | 20 (14.6) | 69 (46.3) | 0.3 | 1.03 |
| ACE-I/ARB | 30 (21.9) | 70 (46.9) | 0.42 | 0.64 |
| Diuretics | 5 (3.6) | 71 (47.6) | <0.0001 | 18.62 |
| Alpha blockers | 1 (0.72) | 8 (5.3) | - | - |
| Clonidine | 3 (2.1) | 27 (18.1) | 0.03 | 4.59 |
| Total units | 137 | 374 | - | - |
Figures in parenthesis indicate percentage. CCBs: Calcium channel blockers, ACE-I/ARB: Angiotensin-converting enzyme inhibitors/angiotensin 2 receptor blockers
Table 5: Pattern of antihypertensive drug use on the basis of type of therapy
Utilization of antihypertensive drugs in comorbid conditions
Table 6 depicts comorbid conditions associated with hypertensive patients and antihypertensives drug therapy. Most common comorbidities included diabetes (44.7%), ischemic heart disease (27.2%), and renal parenchymal disease (20.2%). The CCBs were the most commonly used class of antihypertensives across all comorbidities excluding left ventricular dysfunction/congestive cardiac failure (CCF), in which the diuretics have been used the most (93.7%). Frequency of use of CCBs was 87.5% in asthma/chronic obstructive pulmonary disease (COPD). The use of ACE-I/ARB was 41.4% in diabetes and 34.4% in renal parenchymal disease. Two patients out of a total of 24 having asthma/COPD were prescribed beta blockers (atenolol and nebivolol).
| Comorbid disease | Antihypertensive drug class, n (%) |
|---|---|
| Diabetes (n=128) | CCBs - 83 (64.8) |
| Beta blockers - 43 (33.6) | |
| ACE-I/ARB - 53 (41.4) | |
| Ischemic heart disease (n=78) | Diuretics - 37 (28.9) |
| CCBs - 57 (73) | |
| Beta blockers - 29 (37.1) | |
| ACE-I/ARB - 33 (42.3) | |
| Diuretics - 32 (41) | |
| Renal parenchymal disease (n=58) | CCBs - 46 (79.3) |
| Beta blockers - 19 (32.7) | |
| ACE-I/ARB - 20 (34.4) | |
| Diuretics - 28 (48.2) | |
| Cerebrovascular accident (n=27) | CCBs - 19 (70.3) |
| Beta blockers - 8 (29.6) | |
| ACE-I/ARB - 7 (26) | |
| Diuretics - 5 (18.5) | |
| Left ventricular dysfunction/CCF (n=16) | CCBs - 8 (50) |
| Beta blockers - 12 (75) | |
| ACE-I/ARB - 7 (44) | |
| Diuretics - 15 (93.7) | |
| Dylipidemia (n=22) | CCBs - 14 (63.6) |
| Beta blockers - 9 (41) | |
| ACE-I/ARB - 9 (41) | |
| Diuretics - 6 (27.2) | |
| Asthma and COPD (n=24) | CCBs - 21 (87.5) |
| Beta blockers - 2 (8.3) | |
| Peripheral vascular disease (n=11) | CCBs - 11 (100) |
| Beta blockers - 3 (27.2) | |
| ACE-I/ARB - 3 (27.2) |
Figures in parenthesis indicate percentage. CCBs: Calcium channel blockers, ACE-I/ARB: Angiotensin-converting enzyme inhibitors/angiotensin 2 receptor blockers, CCF: Congestive cardiac failure, COPD: Chronic obstructive pulmonary disease
Table 6: Pattern of use of antihypertensives in comorbid conditions
Discussion
The WHO defines drug utilization studies as “the marketing, distribution, prescription and the use of drugs in a society, with special emphasis on the resulting medical, social and economic consequences.” Prescription pattern surveys are an important methodological instrument of drug utilization studies, which help provide an in-depth insight into the disease profile of patients and prescribing behavior of clinicians.
In this study, the frequency of hypertension was more in males (63.6%) than in females (36.3%). A relative male preponderance was also observed in other studies. [8,9] However, some studies have reported a relatively higher incidence of hypertension in females than in males. [10,11] The mean age of males (56.5 ± 15.9) was more than that of females (53 ± 19.3). A study done in Bengaluru, [8] in contrast to the findings of this study, observed that the mean age of the male patients was slightly less than that of female patients.
CCBs, both as monotherapy and in combination, have been used most frequently. The share of the CCBs in terms of total number of drugs prescribed is almost twice as much as the second largest antihypertensive group of ACE-I/ARBs. The use of amlodipine as an individual antihypertensive agent far exceeds the utilization of any other single drug. A similar trend of CCB and amlodipine use has also been observed in some other studies. [8,9,12] Advantages of amlodipine such as long duration of action, sustained and consistent blood pressure control with once daily dosing, [13] and improved compliance [14,15] are factors that make it an excellent antihypertensive agent and probably contribute to its predominant utilization. The utilization of diuretics, particularly that of the thiazides, was low (9%) as compared to all the other antihypertensive drug groups. Such underutilization of thiazides has been observed across many studies [10,16] despite being recommended as the first choice antihypertensive consequent to their ability to prevent major cardiovascular events [17,18] and low cost. The relatively less frequent use of thiazides could be a result of concerns regarding adverse effects and poor market availability. [19]
Gender-based differences in pattern of antihypertensive use were not significant. Although methyldopa has been recommended as the antihypertensive drug of choice in pregnant women [20] and is also included in the list of essential medicines, it has not been used for the treatment of pregnant hypertensive women. Diuretics and the ACE-I/ARBs, which are contraindicated in pregnancy due to their deleterious effects on the fetus, have been avoided in this group of patients.
The enhanced use of combination therapy (51.1%) as compared to monotherapy (48.8%) in this study is consistent with the JNC7 Report which states that most hypertensive patients with diabetes or renal disease will require two or more antihypertensive drugs to achieve the target blood pressure [21,22] of <130/85 mm Hg. Since large number of patients were suffering from concomitant ischemic heart disease, diabetes, and renal disorders, they are likely to have required multiple antihypertensives to achieve optimal blood pressure control and impede end organ damage. Higher use of combination antihypertensive drug therapy in relation to monotherapy is similar to a study done in Chandigarh [16] where approximately 46% patients received monotherapy and 54% patients received combination therapy. The findings are however different in studies done in India [10,23] and Ethiopia [24] where the use of monotherapy exceeded that of combination therapy. Variation in the frequency of patients having comorbidities observed in some of the other studies could be a reason for the predominant use of a single antihypertensive agent.
The British Hypertension Society Guidelines [25] recommends the use of ACE-I/ARBs or beta blockers in younger hypertensives (higher renin levels) and CCBs or diuretics for elderly (lower renin levels). In this study, the pattern of use of the beta blockers (more in younger hypertensives) and diuretics (more in elder hypertensives) was consistent with guideline recommendations, but pattern of use of the CCBs (slightly more in younger hypertensives) and ACE-I/ARBs (more in elder hypertensives) did not vary accordingly. Consideration of comorbid conditions seems to take precedence over age-related factors while selecting an appropriate antihypertensive. The use of CCBs in elderly hypertensives is concordant with other studies [26,27] and the overall antihypertensive prescribing trend observed in this study.
The utilization of the ACE-I/ARBs in comorbid diabetes was 41.4%, which was less than that of CCBs and beta blockers. This is in contrast to studies done in North India where there has been a predominant use of the ACE-I and/or ARBs in hypertensive diabetics. [16,23,28] ACE-I-based therapy has been recommended to be an integral component of any antihypertensive regimen in patients with diabetes [29,30] and renal disease. [31] Lower frequency of their use in this subgroup of patients is thus in contrast to the recommended guidelines. Higher cost of this antihypertensive class could possibly account for their relatively lower utilization. It is imperative to make pragmatic assessments of cost versus benefit before selecting any therapeutic agent so that the patient is not deprived of the best available therapeutic option. Verapamil has been rightly avoided in CCF because of its cardio depressant properties and nonselective beta blockers have been avoided in bronchial asthma. Most patients suffering from bronchial asthma have been given CCBs. However the cardioselective beta blockers atenolol and nebivolol, have been prescribed in two patients. The cardioselective beta-blockers are associated with a relatively lower risk of bronchoconstriction. Their use in comorbid bronchospastic disease could thus be considered to be appropriate if the potential benefit to the patient outweighs the risk of deleterious adverse effects.
The NLEM is aimed at promoting rational use of medicines by considering their cost, safety, and efficacy, thus prioritizing availability of affordable quality medicine at all levels of healthcare. Compliance with the NLEM in this study was 65% which is lower than that of 90% observed in another study. [16] The use of essential medicines is an important indicator of rational drug use, and emphasis should be laid on their availability and optimal utilization.
Conclusion
The use of antihypertensives in this tertiary care hospital largely conforms to the recommended treatment guidelines. Aspects that need to be seen critically include the underutilization of drugs from the NLEM in general and thiazides in particular as well as the apparent suboptimal use of ACE-I/ARB in diabetes. Evidence-based medicine should be an essential component of continuing medical education to enable advances in clinical research to be translated into best possible patient care practices. Rational drug use should be prioritized in all hospitals, and essential drug list should be well publicized.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005;365:217-23.
- Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens 2014;32:1170-7.
- Gupta R, Gupta VP. Hypertension epidemiology in India: Lessons from Jaipur Heart Watch. Curr Sci 2009;97:349-55.
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224-60.
- National High Blood Pressure Education Programme. The sixth report of the Joint National Committee on Prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med 1997;157:2413-46.
- National High Blood Pressure Education Programme. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA 2003;289:2560-72.
- Kabir Z, Feely J, Bennett K. Primary care prescribing patterns in Ireland after the publication of large hypertension trials. Br J Clin Pharmacol 2007;64:381-5.
- Xavier D, Noby M, Pradeep J, Pais P. Pattern of drug use in hypertension in a tertiary hospital: A cross sectional study in the in-patient wards. IJP 2001;33:456-7.
- Rachana PR, Anuradha HV, Shivamurthy MC. Anti hypertensive prescribing patterns and cost analysis for primary hypertension: A retrospective study. J Clin Diagn Res 2014;8:19-22.
- Tiwari H, Kumar A, Kulkarni SK. Prescription monitoring of anti-hypertensive drug utilisation at the Panjab University Health Centre in India. Singapore Med J 2004;45:117-20.
- Beg MA, Dutta S, Varma A, Kant R, Bawa S, Anjoom M, et al. A study on drug prescribing pattern in hypertensive patients in a tertiary care teaching hospital at Dehradun, Uttarakhand. Int J Med Sci Public Health 2014;3:922-6.
- Catic T, Begovic B. Outpatient antihypertensive drug utilization in Canton Sarajevo during five years period (2004-2008) and adherence to treatment guidelines assessment. Bosn J Basic Med Sci 2011;11:97-102.
- 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines Subcommittee. J Hypertens 1999;17:151-83.
- Parati G, Pomidossi G, Albini F, Malaspina D, Mancia G. Relationship of 24-hour blood pressure mean and variability to severity of target-organ damage in hypertension. J Hypertens 1987;5:93-8.
- Frattola A, Parati G, Cuspidi C, Albini F, Mancia G. Prognostic value of 24-hour blood pressure variability. J Hypertens 1993;11:1133-7.
- Malhotra S, Karan RS, Pandhi P, Jain S. Pattern of use and pharmacoeconomic impact of antihypertensive drugs in a North Indian referral hospital. Eur J Clin Pharmacol 2001;57:535-40.
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981-97.
- Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, et al. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA 1997;277:739-45.
- Malhotra S, Pandhi P. Availability of thiazide diuretics in Chandigarh. J Assoc Physicians India 2000;48:943.
- Brown MA, Whitworth JA. Pregnancy. In: Bennett WM, McCarron DA, editors. Contemporary Issues in Nephrology: Pharmacology and Management of Hypertension. Vol. 28. New York: Churchill Livingstone; 1994. p. 89-116.
- Cushman WC, Ford CE, Cutler JA. Success and predictors of blood pressure control in diverse North American settings: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich) 2002;4:393-404.
- Black HR, Elliott WJ, Neaton JD, Grandits G, Grambsch P, Grimm RH Jr., et al. Baseline characteristics and early blood pressure control in the CONVINCE trial. Hypertension 2001;37:12-8.
- Jhaj R, Goel NK, Gautam CS, Hota D, Sangeeta B, Sood A, et al. Prescribing patterns and cost of antihypertensive drugs in an internal medicine clinic. Indian Heart J 2001;53:323-7.
- Shukrala F, Gabriel T. Assessment of prescribing, dispensing, and patient use pattern of antihypertensive drugs for patients attending outpatient department of Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia. Drug Des Devel Ther 2015;9:519-23.
- Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): Summary. BMJ 2004;328:634-40.
- Mohd AH, Mateti UV, Konuru V, Parmar MY, Kunduru BR. A study on prescribing patterns of antihypertensives in geriatric patients. Perspect Clin Res 2012;3:139-42.
- Lim KK, Sivasampu S, Khoo EM. Antihypertensive drugs for elderly patients: A cross- sectional study. Singapore Med J 2015;56:291-7.
- Dhanaraj E, Raval A, Yadav R, Bhansali A, Tiwari P. prescription pattern of antihypertensive agents in T2DM patients visiting tertiary care centre in North India. Int J Hypertens 2012;2012:520915.
- Hanson L, Lindholm LH, Niskansen L, Lanke J, Hedner T, Niklason A, et al. Effect of angiotensin converting enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: Captopril Prevention Project (CAPP) randomised trial. Lancet 1999;353:611-6.
- Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000;342:145-53.
- Taal MW, Brenner BM. Renoprotective benefits of RAS inhibition: From ACEI to angiotensin II antagonists. Kidney Int 2000;57:1803-17.