Study of Medication Prescribed and Appropriateness of Antimicrobials in Hospitalized Respiratory Tract Infectious Children in Tertiary Care Teaching Hospital, Western Nepal
2 Kaski Sewa Hospital, Pokhara, Nepal
3 Shradha Institute of Health Science, Nepal
4 Western Academy of Health Science, Nepal
5 Department of Clinical Pharmacology and Therapeutics, BPKHIS, Dharan, Nepal
6 Pokhara University, Pokhara, Nepal
Citation: Dhakal SR, Kafle B, Udas B, Duwadi P, Poudel R, Palikhe R, Alam K, Khan GM. Study of Medication Prescribed and Appropriateness of Antimicrobials in Hospitalized Respiratory Tract Infectious Children in Tertiary Care Teaching Hospital, Western Nepal. J Basic Clin Pharma 2018;9:pp-pp.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Background: Respiratory Tract Infection (RTI) is the global cause of death in children. Nepal, India, Indonesia and Bangladesh account 40% of the global cause. Antimicrobials are the most commonly prescribed drugs in hospitals whose appropriateness solely relies on its rational use. Methods: A cross-sectional study was carried out in pediatric in-patients suffering from the respiratory infection at a tertiary care teaching hospital. WHO/INRUD prescribing indicators and appropriateness index were used in determination of the drug prescribing indicators and appropriateness of antimicrobials. Results: A total of 108 samples male incidence were higher than female. The maximum samples were found in between the age group 1-5 years. Brahaman and Chhetri were the found in larger frequency. Bronchopneumonia 67 and Acute Bronchiolitis 21 (19.4%) were the most common diagnosis. Cefotaxime was the drug found to be used in maximum number 81 (54.4%) following Gentamicin and Amoxy-Clav. In 58 (53.7%) sample Cephalosporin were used as single drug, following its combination with aminoglycosides 20 (18.6%) Out of which cefotaxime and gentamicin combination was found to be in 15 samples. In discharged medication 70.3% of the samples were prescribed with Cephalosporin. The average no of drug per prescription were found to be 4.31. 7.7% of the drugs were found to be prescribed in generic name. The antibiotic encounter per samples and medication from essential drug list were found to be 100%. Conclusion: Total of 140 antibiotics were assessed for appropriateness where 50 (35.71%) of antibiotics were found to be appropriate and 90 (64.29%) were found to be inappropriate. The average Medication Inappropriateness (MAI) was 3.29. The mean MAI per prescription was found to be 1.69 ± 0.47. 33 (31.43%) of the samples were found to be appropriate and 72 (68.57%) sample were found to be inappropriate.
Keywords
Respiratory tract infection, antimicrobials, appropriateness, inappropriateness, medication appropriateness index
Background
Respiratory tract infections is the worldwide main cause of death in children aging less than 5 years and which produce 8.2% of the total disease burden. In developed countries respiratory tract infections are the leading cause of morbidity, accounted for 20% of medical consultation.[1] The pediatric population comprises of 20-25% of the total world population, and numerous acute and chronic diseases can effect this sub population. Antibiotics are among the most frequently prescribed classes of medications for children.[2] It is estimated that Bangladesh, India, Indonesia and Nepal together account for 40% of global acute respiratory infection mortality.[3] Acute respiratory infection (ARI) is one of the leading causes of childhood morbidity and mortality in Pakistan. To achieve the reduction in the death rate attributed to pneumonia, WHO’s standard ARI case management guidelines were adopted to act in rationalization of the drug use.[4] Children are particularly challenging group of patients when trying to ensure the safe use of medication. Children are challenging groups and the most important target group for the effort aimed at reducing unnecessary antibiotic use as they receive significant proportion of antibiotics.[5] Upper respiratory tract infection (URTI) is considered as one of the major public health problems. The greatest problem for developing countries is the mortality from URTI in children less than five year of age.[6] Common cold, sore throat, croup, bronchiolitis, pharyngotonsillitis and pneumonia are the common respiratory infection. WHO recognized respiratory diseases as the second important cause of death for children under five years in 2010. [7] Antibiotic are precious but non-renewable resources which are of major benefit to people who have serious and life threatening bacterial infections. Squandering this resources use 97% agreed that “overuse of antibiotics is a major factor contributing to the development of antibiotic resistance.” Prior antibiotic use increases the risk that a child will develop a resistant infection” 78% and that “resistance has resulted in treatment failure for children with URIs are 69%.[8,9] The inappropriate use of antibiotics alarms a significant global public health problem. Inappropriate prescription by both the trained and untrained health care workers where no proven benefit of the therapy may lead to the microbial resistance.[10,11]
Improved patient understanding of the etiology of these infections, and improved compliance where antibiotic therapy is indicated, are of paramount importance.[12] In the developing world effective health care interventions are underutilized, and income-related disparities in use are found in lager extend. Antibiotic drug overuse and inappropriate antibiotic drug selection are associated with increased drug resistance among respiratory pathogens which results in increased treatment costs.[13] Awareness of clinical manifestations that help differentiate viral from bacterial infection and the use of guidelines can promote the appropriate management of respiratory tract infections.[14]
One of the research found out that 16% of antibiotic were prescribed in upper respiratory tract infection, pneumonia and cough/bronchitis were prescribed with 78% and 28% respectively in each of the cases. [15] Regarding the cost Antimicrobials are among the most commonly prescribed drugs in hospital that account for over 50% of total value of drugs sold in the country.[16] Over prescribing of antibiotics Sociocultural and economic pressures, Malpractice litigation concerns: there is a rapid course for some bacterial diseases that are preceded by viral illness and patients may not return if illness worsens or persists and meeting parent expectations: dissatisfied parents may seek care elsewhere[17] “Prior antibiotic use increases the risk that a child will develop a resistant infection” 78% and that “resistance has resulted in treatment failure for children with URIs are 69%.[9] Prudent antibiotic use is only option to delay the development of resistance, because of few new antibiotics in the Research and Development.[18]
Methods
Study design
A cross-sectional study was conducted in which patients taking medication during the treatment were observed.[19,20]
Study site
The study was conducted Manipal Teaching Hospital (MTH) a 700 bedded multidisciplinary tertiary care teaching hospital located in Pokhara City, western Nepal. Average of 500 outpatients visit hospital per day and with about 250 bed occupancy.[21]
Study setting
The study was conducted in the pediatric inpatient of Manipal Teaching Hospital. Entire patient admitted in the pediatric ward for treatment of respiratory tract infection were taken. Antimicrobial prescribed for the treatment of respiratory tract infection for children will be taken in considerations.
Study duration
The Study was carried out for period of six month which included time for the literature review, data collection and data analysis. The actual time for data collection was ten weeks.
Sampling techniques
The prescriptions were taken and/or the details were followed till discharge of the patients. The data for present study was collected by chart review method. During the study inpatients case records was reviewed, which included patients case history, diagnosis, physician medication order sheets, nurse medication administration records, progress chart, laboratory investigations and report of other diagnostic tests. This information was documented in the patient profile form. All the prescription documented were analyzed for following parameters such as demographic status of patients, disease diagnosis, the medication used during the treatment, appropriateness of antimicrobials and assessment of cost. All data are represented in percentage.
Sample size
Sample size is calculated by using the formulae (WHO, 2001) where,
N=Z2p (1-p)/D2
Where, N=approximate sample size; Z=Z value at a given confidence interval; D=Margin of error.
Inclusion and exclusion criteria
All the Respiratory inpatients in pediatric ward of Manipal Teaching Hospital, Phulbari, Pokhara, Nepal, were taken. Critically ill, patients receiving antimicrobial from out-patient pharmacy, children below one year and other admitted pediatric patients beside respiratory illness were excluded. The patients transferred to ICU were not further followed.
Data collection
Data were collected after obtaining written consent), using patient profile form which included demographic status of patients, disease diagnosis, the medication used during the treatment, appropriateness of antimicrobials and assessment of cost for the period of ten weeks. Patient those transferred to ICU during the study period were not followed.
Criteria and methods for data collection
The Criteria for assessing used was the WHO/INRUD prescribing indicators and medication appropriateness index the tool developed by Hanlon et al. and Samsa et al.[22,23] was used after the permission being granted which consists of ten purviews: indication, effectiveness, dosage, correct directions, practical directions, drug-drug interactions, drug-disease interactions, duplication, duration and expense. The assessment of antibiotics appropriateness was done by the committee formed which consists of a group of physician and clinical pharmacist. Regarding the guideline Clinical practice guidelines on pneumonia and respiratory tract infections in children was used (URL-1).
Data collection tools
These tools are the self-developed forms that are used to document the evidence during the research procedure. Descriptive analysis was done by using SPSS Version 20. The ethical approval for the research was obtained from Ethical Research Board of Manipal Teaching Hospital.
Results
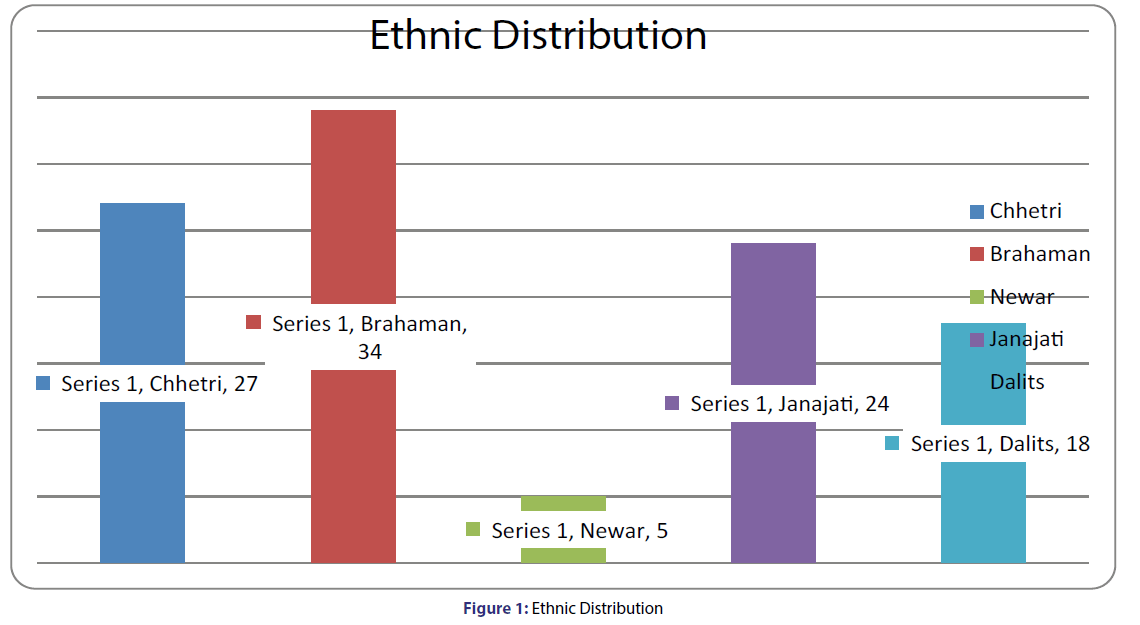
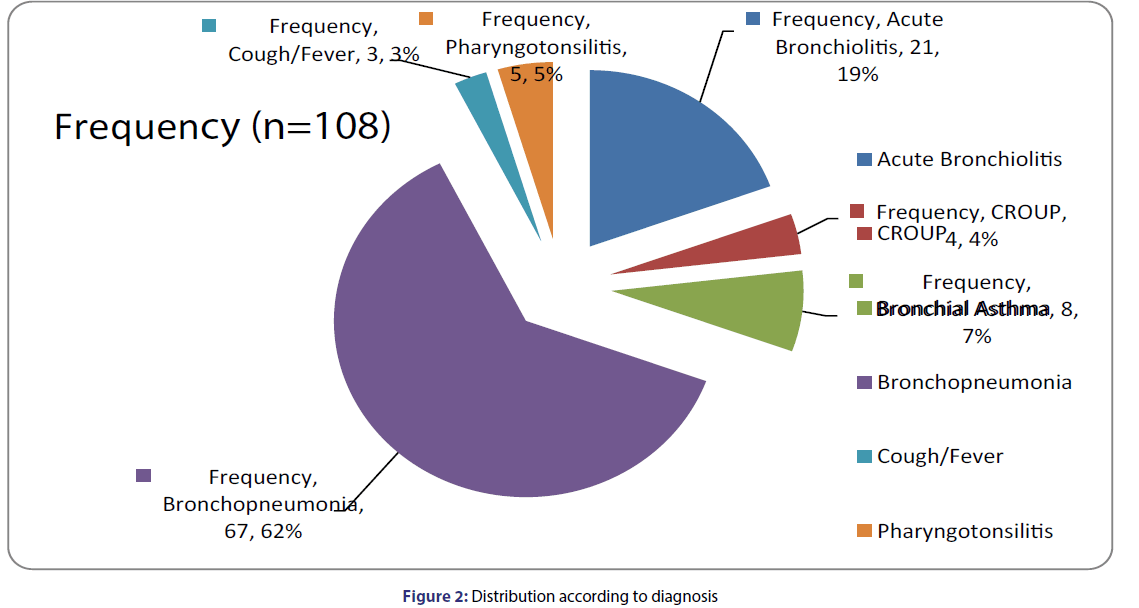
A total of 108 samples who met the inclusion criteria were selected and were followed for the present study. The cases were analyzed bases upon the following parameters. Among 108 total samples taken for the study 65 (60.2%) were male and 43 (39.8%) were female [Table 1]. The highest range includes age group in-between 1-5 years i.e., 92% following the age group 6-10 years. The lowest no ranges in-between the age group 11-15 years [Table 2]. The mean age was found to be 2.5975 ± 2.64364. Brahaman 34 (31.5%) were found to be the highest frequency following Chhetri 27 (25%), Janajati 24(22.2%), Dalit 18 (16.7%) and Newar 5 (4.6%) respectively [Figure 1]. The most commonly diagnosed case out of 108 samples was bronchopneumonia, 64 (62%), following Acute Bronchiolitis 21 (19.4), Bronchial Asthma 8 (7.4%) Pharyngotonsilitis 5 (4.6%), CROUP 4 (3.7) and Cough along with fever 3 (2.8%) [Figure 2].
| Gender | Total Sample | Percent |
|---|---|---|
| Male | 65 | 60.2 |
| Female | 43 | 39.8 |
| Total | 108 | 100 |
Table 1: Demographic Status of the patients
| Age Group (Years) | Frequency | Percent |
|---|---|---|
| 1-5 | 92 | 85.2 |
| 6-10 | 13 | 12 |
| 11-15 | 3 | 2.8 |
| Total | 108 | 100.0 |
Table 2: Age-wise distribution
Antibiotic used during stay
A total of 149 antibiotics were found to be used, out of which Cefotaxime was found to be the drug used in highest frequency i.e., 81 (54.5%) following by the gentamycin 20 (13.4%). Cephalosporin (92 (62%)) was the antibiotic found to be used in larger number following Aminoglycosides and Penicillin antibiotics, 27 (18%) and 24 (16.1%) respectively. Each sample consists of 1.38 ± 0.62 antibiotics and 1.367 ± 0.99 injections [Table 3].
| Antibiotic | Frequency | Percentage |
|---|---|---|
| Cefotaxime | 81 | 54.4 |
| Cefpodoxime | 2 | 1.3 |
| Cefixime | 1 | 0.7 |
| Ceftriaxone | 5 | 3.4 |
| Flucloxacillin | 2 | 1.3 |
| Ceftazidime | 3 | 2.0 |
| Amoxy-Clav | 13 | 8.7 |
| Ampicillin | 9 | 6.1 |
| Azithromycin | 2 | 1.3 |
| Gentamycin | 20 | 13.4 |
| Vancomycin | 2 | 1.3 |
| Amikacin | 4 | 2.7 |
| Mupirocin | 3 | 2.0 |
| Tobramicin | 1 | 0.7 |
| Ciprofloxacin | 1 | 0.7 |
| Total | 149 | 100 |
Table 3: Antibiotic used during the stay
No of antibiotic used
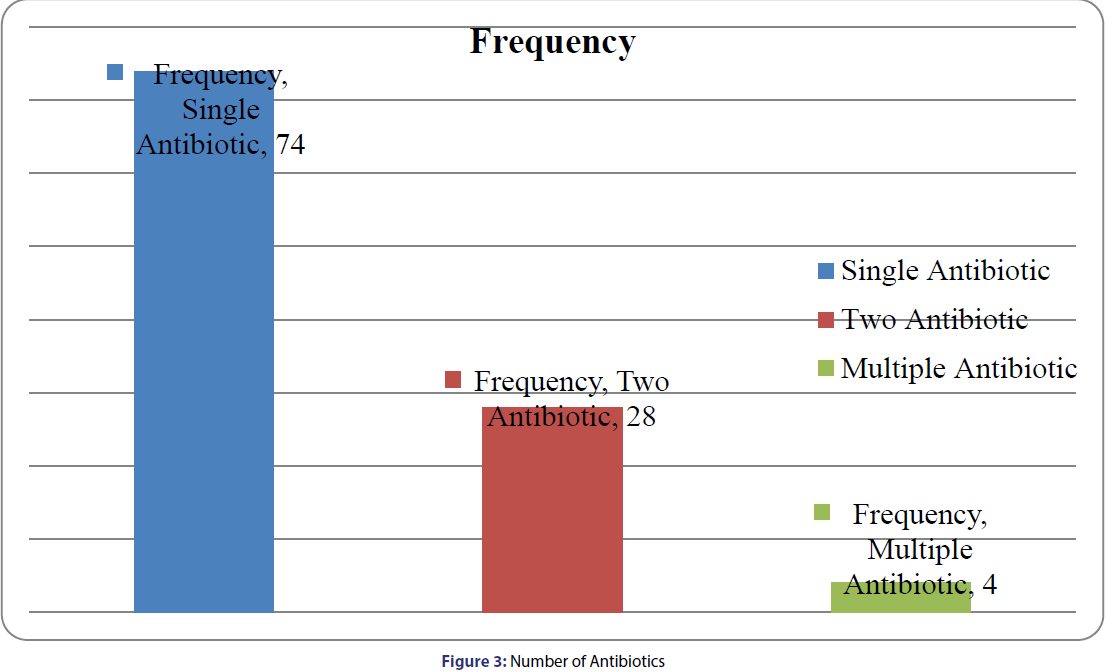
Out of the total sample 108, 74 (68.5%) consist of single antibiotic whereas 28 (25.9%) were prescribed with two antibiotics. Similarly, 4 prescriptions were found prescribed with multiple antibiotics [Figure 3]. Table 4 explains that the Combination of Cephalosporin and Aminoglycoside found to be used in greater amount i.e., 20 (22.2%) of the total patient prescription.
| Antibiotic Group | Frequency | Percentage |
|---|---|---|
| Cephalosporin | 58 | 53.7 |
| Penicillin | 18 | 16.7 |
| Cephalosporin+Aminoglycosides | 20 | 18.6 |
| Cephalosporin+Macrolides | 2 | 1.8 |
| Cephalosporin+Penicillin | 2 | 1.8 |
| Cephalosporin+Monocarboxyllic Acid | 3 | 2.8 |
| Penicillin+Aminoglycoside | 3 | 2.8 |
| Cephalosporin+Aminoglycosides+Penicillin | 1 | 0.9 |
| Cephalosporin+Aminoglycosides+Fluoroquinolones | 1 | 0.9 |
| Total | 108 | 100 |
Table 4: Group of Antibiotic used
Other medications prescribed during stay
A total of 316 medications beside antibiotics were found to be used during the study period. Out of which Inhalant, NSAIDs were used in large no of patients [Table 5].
| Other Medication | Frequency | Percentage |
|---|---|---|
| Inhalant | 103 | 95.4 |
| Metered Dose Inhaler | 4 | 3.7 |
| Anti-histamine | 5 | 4.6 |
| Corticosteroid | 13 | 12 |
| H2-Blockers | 16 | 14.8 |
| Local Applicant | 5 | 4.6 |
| Nasal Decongesant | 20 | 18.5 |
| Anti-Diarrhoeal | 13 | 7.4 |
| Cough Suppressant | 11 | 10.2 |
| NSAIDs | 95 | 88 |
| Anti-emetic | 7 | 6.5 |
| Others | 24 | 22.2 |
Table 5: Others medication during stay
Antibiotic on discharge
Single drug antibiotic was found to be used in all of the cases were cephalosporin 76 (70.30%) being the highest no of prescription followed by penicillin antibiotic and 16 (14.8%) respectively. Out of remaining ten samples three of them were transferred to intensive care unit and remaining seven parents’ opted to take their child home at their own risk [Table 6].
| Antibiotics | Frequency | Percentage |
|---|---|---|
| Cefpodoxime | 67 | 62 |
| Ampicillin | 1 | 0.9 |
| Amoxicillin | 7 | 6.5 |
| Amoxy-Clav | 8 | 7.4 |
| Cefixime | 8 | 7.4 |
| Cefuroxime | 1 | 0.9 |
| No Antibiotic | 6 | 5.6 |
| Total | 99 | 90.7 |
| Left Against Medical Advice | 7 | 6.5 |
| Transferred to ICU | 3 | 2.8 |
Table 6: Antibiotic on discharge
The average number of drug per prescription was found to be 4.31 ± 1.51. Higher than that of WHO/INRUD standard. Similarly 7.7% of the drugs were found to be prescribed by generic name. The percentage of encounter prescribed as injection was found to be 38.71%. All the samples were found to be prescribed with antibiotic [Table 1]. The medication appropriateness was determined by the committee of health professionals including doctors and clinical pharmacists. Out of the total 140 antibiotic accessed 50 (35.71%) of antibiotics were found to be appropriate whereas remaining 90 (64.29%) of the antibiotics were found to be inappropriate. The average MAI score was found to be 3.29. Mean MAI per Prescription was found to be 1.69 ± 0.47. Overall sample appropriateness was found to be 33 (31.43%) and inappropriateness was found to be 72 (68.57)% [Tables 7 and 8].
| Prescribing Indicator | Result | WHO/INRUD Standard |
|---|---|---|
| Average no of drug per prescription | 4.31 ± 1.51 | ≤ 3 |
| Percentage of drug prescribed by generic name | 7.7% | 100% |
| Percentage of encounters with injections | 38.71% | ≤ 10% |
| Percentage of patient encounters with an antibiotic prescribed. | 100% | ≤ 30% |
| Percentage of drugs prescribed from the national EDL or the facility’s formulary. | 100% | 100% |
Table 7: WHO/INRUD Prescribing Indicator
| Criteria | Appropriateness | Marginally Appropriate | Inappropriate | MAI |
|---|---|---|---|---|
| Indication | 124 | 3 | 13 | 42 |
| Effectiveness | 89 | 45 | 6 | 63 |
| Correct Dosage | 78 | 33 | 29 | 91 |
| Correct Direction | 138 | 2 | 2 | |
| Practical | 119 | 10 | 11 | 32 |
| Drug-Drug Interaction | 126 | 0 | 14 | 28 |
| Drug-Disease Interaction | 140 | 0 | 0 | |
| Duplication with other drug | 131 | 0 | 9 | 9 |
| Duration of therapy | 113 | 0 | 27 | 27 |
| Expensiveness | 110 | 0 | 35 | 35 |
| Average Score | 11.48 | 9.3 | 1.39 | 3.29 |
Table 8: Appropriateness on antibiotics
Discussion
The number of male incidence was found to be higher in the study 65 (60.2%). Similar result was seen in the research done by Rijal et al. and Munir[24,25] where the incident of male were found to be 58.1% and 64.2% respectively. The highest percentage of age group being affected were found to be in-between 1-5 years of age i.e., 85.2%. In another research done by Duarte et al.[26] found to be 52.1%. Although impact being the same. The higher incidence of male greater than female is explained by NIPORT 2005, as may be due to genetic or there may be higher reporting for boys due to gender bias where mothers may be considering it more serious for boys or it is considered less serious for girls.
There is also evidence that women receive different care than men for common chronic disorders, while they make more visits to physicians for acute, self-limited diseases. Nevertheless, females live longer than males in most populations.[27] The discrepancy in distribution of respiratory tract infection among various ethnic groups could be attributed to their social, cultural and religious background not mentioning the inequality in access to services and in the range of opportunities available.[28] Maigolis et al. suggests that there is evidence that highly educated families are more likely than less-educated families to report respiratory symptoms. It also indicate that much of the effect of socioeconomic status can be explained by factors that are related to the infant’s home environment, most of which are mutable (exposure to tobacco smoke, crowding, stress, low birth weight, and bottle feeding). In addition, exposure to risk factors for respiratory illness is not only more common among families of low socioeconomic status, but the effect of the exposure also seems to be the greatest in this group, at least among infants not in day care.[28]
A total of 149 antibiotics were found to be used in the study during the treatment phase. Where, Cephalosporin 53.7% was the drug found to be used in most of the cases following its combination with aminoglycosides 18.6% and penicillin 16.7% respectively. Cephalosporins were the most often prescribed class of antimicrobials (56.36%) followed by Penicillins (40.36%) and Aminoglycosides (36.36%). Injection was the commonest route of administration (58.25%). Lower respiratory tract infection was the commonest diagnosis[29] by Ramesh et al. Another research showed that Cephalosporin 92 (62%) was the antibiotic found to be used in larger number following Aminoglycosides and Penicillin antibiotics.[30] Broad-spectrum antibiotics were the most commonly prescribed antibiotic class in hospitals, namely third generation Cephalosporin.[31] Pneumonia was the most prevalent diagnosis among infant. During the treatment the combination of aminoglycosides and cephalosporin was found to be 20 (18.6%) out of which 15 (75)% of this combination consists of Cefotaxime and Gentamicin. Similar result was seen in study by other scholars.[32]
The average MAI score obtained was 3.29. Out of the total 140 antibiotic accessed 50 (35.71%) of antibiotics were found to be appropriate whereas remaining 92 (64.29%) of the antibiotics were found to be inappropriate. In total sample done for determination of appropriateness, the mean MAI was found to be 1.69 ± 0.47, where 33 (31.43%) were found to be appropriate and remaining 72 (68.57%) were found inappropriate. In another study the rate of indication appropriateness for inpatients was 1637/2070 (79.0%). Inappropriate dosing which encountered in internal ward being a result of failing to tailor pharmacotherapy for each individual.[33] Another results indicated that 56.3% of total patients on antimicrobials were judged as inappropriate (56.8% with antimicrobial therapy and 55.9% with antimicrobial prophylaxis).[34] In one of the study provide information that even though prescribing practices has improved, a high rate of inappropriate antibiotic prescribing continues. Almost half of patients with upper respiratory tract infections receive antibiotics.[35] In a research done by West et al.[36] a total of 3131 drugs (44.9%) were considered to be appropriate out of which 56 drugs were marginally appropriate, whilst 55.1% (n=384) of drugs were prescribed inappropriately, i.e., 55.1% of drugs met one or more criteria of the MAI. The results of this study show that 55.1% of the drugs prescribed during this study, based on MAI criteria, were inappropriate for one reason or another. In one of the research done in Nepal the appropriateness of antimicrobial was found to be 31.7%.[37]
Limitation of the study
►The research was carried out for the short duration of time period.
►Children below one year were not taken in the study.
►Due the absence of the standard treatment guideline, the guideline validated by the physicians was taken in consideration.
►The research was carried out in only one pediatric inpatient of a hospital. Therefore the result might not be extrapolated to the other teaching hospital.
Conclusion
Prescribing higher generation antibiotics and duplication with antibiotics were common types of inappropriateness. Similarly antibiotics alone account 76.08% of the medication cost. 50 (35.71%) of antibiotics were found to be appropriate and 90 (64.29%) were found to be inappropriate. The average Medication Inappropriateness (MAI) was 3.29. The mean MAI per prescription was found to be 1.69 ± 0.47. 33 (31.43%) of the samples were found to be appropriate and 72 (68.57%) sample were found to be inappropriateness. The use of antimicrobial was found to be prescribed in 100% of the cases of Respiratory Tract Infection. The cases of inappropriateness were found to be higher than that of appropriateness which shows the requirement in improvement in rationalization of antibiotics.
Abbreviations
ARI: Acute Respiratory Infection; RTI: Respiratory Tract Infection; URTIs: Upper Respiratory Tract Infections; LRTIS: Lower Respiratory Tract Infections; CXR: Chest Radiography; GERD: Gastro esophageal Reflux Disease; GAS: Group-A Streptococcus; CAP: Community Acquired Pneumonia; HAP: Hospital Acquired Pneumonia; NSAIDs: Non-Steroidal Anti Inflammatory Drug; RSV: Respiratory Syncytial Virus; WHO: World Health Organization; INRUD: International Network for Rational Use of Drugs; MTH: Manipal Teaching Hospital; US: United States.
REFERENCES
- Gutiérrez-Tarango MD, Berber A. Safety and Efficacy of Two Courses of OM-85 BV in the Prevention of Respiratory Tract Infections in Children During 12 Months. Chest 2001;119:1742-8.
- Mishra H, Mishra R, Mondal A. Prescription pattern of antimicrobial drugs in pediatrics outpatient department of a tertiary care teaching hospital of North India. Int J Basic and Clinical Pharmacol 2014;3:1.
- Duwadi S. Pattern of antimicrobial prescription and its cost analysis in respiratory tract infection. Kathmandu University J Sci 2005;1:1-9.
- Quazi SA, Rehman GN, Khan M. Standard management of acute respiratory infections in a children's hospital in Pakistan:impact on antibiotic use and case fatality. Bulletin of the World Health Organization 1996;74:501-7.
- Khalil GM, Alghasham AA, Abdelraheem YF. Effect of Establishment of Treatment Guidelines on Antibiotic Prescription Pattern for Children with Upper Respiratory Tract Inf Life Sci. J 2012;9:481-6.
- Prabhakar TS, Vital Rao NS. A Study on Antibiotic Prescriptions for Upper Respiratory Tract Infection (Urtis) in Childrens at a Tertiary Care Teaching Hospital. Res J Pharmaceuti Biolo and Chem Sci 2015;6:813-9.
- Boloursaz MR, Lotfian F, Aghahosseini F, Cheraghvandi A, Khalilzadeh S, Farjah A, et al. Epidemiology of Lower Respiratory Tract Infections in Children. J Comprehensive Pediatri 2013;4:93-8.
- JEETACAR. The use of antibiotics in food-producing animals. Commonwealth of Australia 1999.
- Watson RL, Scott F, Dowell D, Jayaraman M, Keyserling K, Kolczak M, et al. Antimicrobial Use for Pediatric Upper Respiratory Infections: Reported Practice, Actual Practice, and Parent Beliefs. Pediatri 1999;104:1251-9.
- Wutzke SE, Artist MA, Kehoe LA, Fletcher M, Mackson JM, Weekes LM, et al. Evaluation of a national programme to reduce inappropriate use of antibiotics for upper respiratory tract infections: effects on consumer awareness, beliefs, attitudes and behaviour in Australia. Health Promot Int 2007;22:53-64.
- Alumran A, Hurst C, Hou XY. Antibiotics Overuse in Children with Upper Respiratory Tract Infections in Saudi Arabia: Risk Factors and Potential Interventions. Clinical Med Diagno 2012;1:8-16.
- Johnston L. Rational use of antibiotics in respiratory tract infections. South African Pharmaceut J 2012;79:34-9.
- O’Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cadernos Saúde Pública, Rio de Janeiro 2007;23:2820-34.
- Thomas MF, Hadley JA. Rational Use of Antibiotics to Treat Respiratory Tract Infections. The Am J Manag Care 2002;8:713-27.
- Akkerman AE, Kuyvenhoven MM, van der Wouden JC, Verheij TJ. Determinants of antibiotic overprescribing in respiratory tract infections in general practice. J Antimicrob Chemother 2005;56:930-6.
- Prajapati V. Study of prescribing patterns of antimicrobial agents in the paediatric wards at tertiary teaching care hospital, Gujarat. Int J Pharmaceuti Sci and Res 2012;3:2348-55.
- Pichichero ME. Understanding antibiotic overuse for respiratory tract infections in children. Pediatri 1999;104:1384-8.
- Gyssens I. Antibiotic policy. International Journal of Antimicrobial Agent 2011;38:11-20.
- Levin KA. Study design III: Cross-sectional studies. Evid Based Dent 2006;7:24-5.
- Barroga EF. Research study designs: an appraisal for peer reviewers and science editors. Eur Sci Editing 2013;39:44-5.
- Dubey A, Palaian S, Shanakar P, Mishra P, Prabhu M, Bhandari RB, et al. Introduction to medication errors and the error prevention initiatives in a teaching hospital in Western Nepal. Pakistan J Pharmaceuti Sci 2006;19:244-51.
- Hanlon JT, Schamader KE, Samsa GP, Weinberger M, Uttech KM, Lewis IK, et al. A Method For Assessing Drug Therapy Appropriateness. J Clinical Epidemiolo 1992;45:1045-51.
- Samsa GP, Hanlon JT, Schmader KE, Weinberger M, Clipp EC, Kim U, et al. A Summated Score For The Medication Appropriateness Index: Development And Assessment Of Clinimetric Properties Including Content Validity. J Clinical Epidemiolo 1994;47:891-6.
- Munir S. Acute Respiratory Infection among Children aged 2 Month to 5 Years: Do Children with Initially “No Pneumonia” Progress to Pneumonia? Annals of Pakistan Institute of Med Sci 2009;5:154-7.
- Rijal P, Shrestha S, Upadhyay S. Profile of acute lower respiratory tract infection in children under fourteen years of age at Nepal Medical College Teaching Hospital (NMCTH). Nepal Med College J 2011;13:58-61.
- Dirce MG, Duarte BC. Clinical profile in children under five year old with acute respiratory tract infections. J de Pediatria 2000;76:207-12.
- Komaroff AL, Robb-Nicholson C, Dunaif A. Women's health Harrison's principles of internal medicine. United Kingdom. McGraw Hill 2001;21-5.
- Peter AM, Robert A, Greenberg M, Keyes LM, Lisa LaVange MP, Robert S, et al. Lower Respiratory Illness in Infants and Low Socioeconomic Status. Am J Public Health 1992;82:1119-26.
- Ramesh L, Sai Sangeeta S, Hussain Y Sr. Analysis of Antimicrobial Prescriptions in Pediatric Patients in a Teaching Hospital. Asian J Pharmaceutical and Clinical Res 2012;5:124-8.
- Kailash T, Shakti S, Sheela B, Damodar B, Chaudhary RK. Prescribing Pattern Of Antibiotics In Pediatric Hospital In Chitwan District In Nepal. World J Pharmacy and Pharmaceutic Sci 2015;4:1631-41.
- Sharma M, Damlin A, Pathak A, Lundborg CS. Antibiotic Prescribing among Pediatric Inpatients with Potential Infections in Two Private Sector Hospitals in Central India. PLoS ONE 2015;10:1-12.
- Palikhe N. Prescribing Pattern of Antibiotics in Paediatric Hospital of Kathmandu Valley. Kathmandu University Med J 2004;2:31-6.
- Forough A, Hosseini S, Jabbari S. Antibiotic utilization evaluation of inpatient and outpatient prescriptions in a rural general hospital in Iran. Int J Basic and Clinical Pharmacol 2015:531-6.
- El-Ashmony SMA. Different Patterns of Inappropriate Antimicrobial Use: A Cross Sectional Study. Life Sci J 2013;10:216-22.
- David RN, Jeffrey H, Ellen RW, Kelleher KJ. Antibiotic Prescribing by Primary Care Physicians for Children With Upper Respiratory Tract Infections. Archives of Pediatrics and Adolescent Med J 2002;156:1114-9.
- Lorna MW, Maria C, Cunningham S. Clinical pharmacist evaluation of medication inappropriateness in the emergency department of a teaching hospital in Malta. Pharmacy Practice 2012;10:181-7.
- Kadir A, Mishra P, Angsulee N. Appropriateness of Antibiotic Use in Enteric fever inpatients in Tertiary Care Hospitals in Western Nepal: A Cross-Sectional Study. Nepal J Epidemiolo 2013;3:236-42.