Rare Manifestation of Digoxin Toxicity: Right Bundle Branch Block
- *Corresponding Author:
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
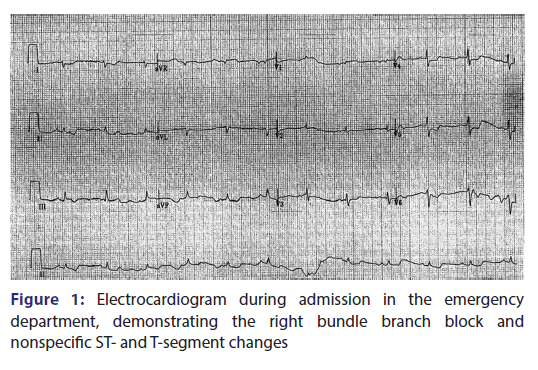
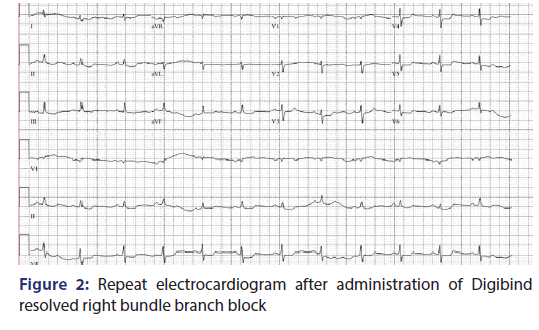
A 76 year old female, with medical history significant for systolic congestive heart failure, who presented to the emergency department with lethargy and abdominal pain with diarrhea for the past 3 weeks. Due to hypotension, the patient received multiple boluses of isotonic saline and was started on norepinephrine. Laboratories were significant for severe digoxin toxicity (29 ng/mL), in setting of acute kidney injury. Electrocardiogram (EKG) revealed a new right bundle branch block (RBBB). She was given Digibind and her repeat digoxin level was 20 ng/mL. Repeat EKG showed resolved RBBB. This case identifies that patients with digoxin toxicity are at risk for RBBB. This is a rare finding and is not commonly recognized. Emergency medicine physicians are often the first to encounter patients with digoxin toxicity and need to be aware of such EKG findings.
Keywords
Digibind, digoxin, right bundle branch block
Introduction
Digoxin is a drug that is mainly used to treat signs and symptoms of atrial fibrillation and mild-to-moderate reduced ejection fraction heart failure. Digoxin works by inhibiting the sodium/potassium ATPase and suppressing the atrioventricular (AV) conduction. [1] Most common significant adverse reactions involve the cardiovascular system, and include accelerated junctional rhythm, atrial tachycardia with or without block, ST segment depression, PR prolongation, and first, second, or third degree AV block. [1] However, we report a rare case of right bundle branch block (RBBB) with serious digoxin toxicity.
Case Report
A 76-year-old female with medical history significant for systolic congestive heart was brought in after she was found to be lethargic and had abdominal pain with diarrhea for 3 weeks. History was limited as patient was somnolent and on venturi mask. In the emergency department, the patient was given four boluses of isotonic saline, but her systolic blood pressure was still ranging in 60–70 mmHg. Hence, central line was placed and norepinephrine was started. Her vitals were remarkable for heart rate of 69 beats/min, respiratory rate of 17 breaths/ min, oxygen saturation of 98% on venturi mask, and blood pressure of 79/42 mmHg on norepinephrine. Physical examination was significant for lethargic appearing female. The right upper chest had inspiratory crackles, and lower extremities had mottled appearance. Laborataries were remarkable for potassium of 8.5 mmol/L, lactic acid of 7.4 mmol/L, bicarbonate of 10 mmol/L, with creatinine of 3.6 mg/dL. Arterial blood gas showed pH of 7.039, CO2 of 44 mmHg, HCO3 of 12 mEq/L, and pO2 of 60 mmHg. Digoxin level was 29 ng/mL. Electrocardiogram (EKG) showed RBBB and nonspecific ST- and T-segment depression [Figure 1]. She was given Digibind for her severe digoxin toxicity and received insulin with dextrose, albuterol, 2 amps (50 meq) of bicarbonate, and calcium gluconate for potassium toxicity. Repeat EKG showed resolved RBBB and improved ST- and T-segment depressions [Figure 2]. Nonetheless, the patient went into bradycardia and then asystole, and expired despite resuscitative efforts. RBBB is extremely rare, Aravanis and Michaelides reported a case of RBBB with atrial flutter.[1] A case of intermittent RBBB due to digitalis toxicity has also been reported.[2] Gould et al. also reported a case of RBBB from digoxin toxicity.[3] Signs of toxicity can occur at doses >2 ng/ mL, and our patient had Digoxin level of 29 ng/mL, which decreased to 20 ng/mL after Digibind was administered.[4-6] Our case demonstrates that the appearance of a new RBBB can be a manifestation of digoxin toxicity. Hence, digoxin toxicity can produce many arrhythmias and RBBB needs to be added on to the list. Emergency room physicians should be vigilant for diagnosing digoxin toxicity in patients that present with classic overdose symptoms, and have new RBBB on EKG reading.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Aravanis C, Michaelides G. Paroxysmal auricular flutter and right bundle branch block following digitalis therapy. Am J Cardiol 1959;4:124-7.
- Sundar S, Avasthey P, Burma DP, Vaish SK. Intermittent right bundle branch blockdue to digoxin toxicity – A rare electrocardiographic manifestation. Indian Heart J 1983;35:238-40.
- Gould L, Patel C, Betzu R, Judge D, Lee J. Right bundle branch block: A rare manifestation of digitalis toxicity – Case report. Angiology 1986;37:543-6.
- Cohen BM. Digitalis poisoning and its treatment. N Engl J Med 1952;246:225-30.
- Lown B, Levine SA. Current concepts in digitalis therapy. Part II. N Engl J Med 1954;250:819-32.
- Flaxman N. Digitoxin poisoning; report of 30 cases. Am J Med Sci 1948;216:179-82.