Quality of prescribing for hypertension and bronchial asthma at a tertiary health care facility, India using Prescription Quality Index tool
- *Corresponding Author:
- Prof. Jalpa V. Suthar
Department of Pharmacology, Ramanbhai Patel College of Pharmacy, Charotar University of Science and Technology, CHARUSAT Campus, Changa, Gujarat, India.
E-mail: jalpasuthar.84@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Objective: Several tools have been introduced to evaluate the quality of prescribing. The aim of this study was to determine the quality of prescribing in hypertension and bronchial asthma in tertiary health care (THC) setting using the new Prescription Quality Index (PQI) tool and to assess the reliability of this tool. Methods: A prospective cross-sectional study was carried out for 2 months in order to assess the quality of prescribing of antihypertensive and antiasthmatic drugs using recently described PQI at THC facility. Patients with hypertension and bronchial asthma, attending out-patient departments of internal medicine and pulmonary medicine respectively for at least 3 months were included. Complete medical history and prescriptions received were noted. Total and criteria wise PQI scores were derived for each prescription. Prescriptions were categorized as poor, medium and high quality based on total PQI scores. Results: A total of 222 patients were included. Mean age was 56 ± 15.1 years (range 4–87 years) with 67 (30.2%) patients above 65 years of age. Mean total PQI score was 32.1 ± 5.1. Of 222 prescriptions, 103 (46.4%) prescriptions were of high quality with PQI score ≥34. Quality of prescribing did not differ between hypertension and bronchial asthma (P > 0.05).The value of Cronbach’s α for the entire 22 criteria of PQI was 0.71. Conclusion: As evaluated by PQI tool, the quality of prescribing for hypertension and bronchial asthma is good in about 47% of prescriptions at THC facility. PQI is valid for measuring prescribing quality in these chronic diseases in Indian setting.
Keywords
Bronchial asthma, hypertension, prescribing quality, Prescription Quality Index tool, rational prescribing
Introduction
Prescribing is a complex phenomenon, with multiple attributes of quality. This complexity can interfere with efforts to improve the quality of pharmacological care that patients receive because improvements in some quality domains can inadvertently cause harm in others. [1] Prescribing quality is an important determinant of wellbeing for older people, and balancing demands for increased effective prescribing with the risk of adverse events is a challenge for primary care. [2]
The large number of candidate indicators of prescribing quality based on register data have been constructed and validated by consensus methods. Few studies have systematically analyzed other validity aspects of these indicators. [3] Indicators are used for a number of different purposes, covering quality management in a broad sense. At the professional level, physicians use indicators for quality development and educational activities, assisting learning processes. [4] They are used by researchers to evaluate interventions, for example in experimental randomized studies testing new methods for changing prescribing behavior. [5] Finally, indicators are increasingly used by administrators of the health system for monitoring quality, screening for quality problems, benchmarking and providing feedback to physicians. [3]
Various measures have been developed to evaluate prescribing quality, e.g. explicit indicators [6,7] like The Medication Appropriateness Index developed by Hanlon et al. [8] at Duke University Medical Centre (Durham, NC, USA) to evaluate the appropriateness of medication use in individual patients, WHO prescribing indicators, [9] and multidimensional indicators. [8,10] The Swedish National Board of Health and Welfare has established explicit indicators for evaluation of drug therapy among elderly patients. [11] However, there is no universal definition of medication appropriateness, because the quality may be assessed in different ways, depending on data available (prescription database vs. individual assessments), setting and comprehensiveness. Most of the measures are based on expert judgment of practitioners or consensus [12-16] without information on the psychometric properties of the instruments. Thus, there is a lack of a single tool that will capture all facets of prescription quality and which is applicable for measurement of prescription quality in chronic diseases, especially those with multiple co-morbidities.
Improvement in prescribing practices can be made by evaluating the quality of prescribing, and any tool that would evaluate all the aspects of prescription right from the selection of the drug to complete prescribing instructions would be more appropriate. Prescription Quality Index (PQI) developed by Hassan et al. in 2010, [17] is the tool intended to evaluate the quality of drug prescribing in chronic diseases. It contains 22 criteria in question form. The PQI has been claimed to be the ideal tool applicable to a broad variety of medications and clinical conditions and easily adopted for application in different settings and limited availability of data. The criteria in the PQI are specifically chosen to measure the common problems related to clinical, clerical and legal requirements of a prescription. [17]
This study aimed to determine the quality of prescribing in patients of two chronic diseases-hypertension and bronchial asthma at a tertiary health care (THC) teaching hospital in Gujarat state of India using the PQI tool [17] and to assess the reliability of this tool.
Methods
This prospective cross-sectional study was carried out for 2 months (April 2013 to May 2013) at medicine and chest medicine outpatient departments (OPDs) at tertiary health facility. Written approval from the Institutional Human Ethics committee was obtained (approved protocol No: HMPCMCE/UG/PG/18/14). Each participant’s informed consent was obtained before collecting his/her data and any relevant information.
Inclusion criteria
Patients of all ages suffering from hypertension and asthma with or without co-morbidities and attending the internal medicine and pulmonary medicine OPDs of a tertiary care teaching facility (THC) for 3 months or longer and ready to give consent were included in the study.
Data collection and evaluation for prescription quality index score
Data were collected for a period of 4 weeks (3 days in a week) at each department (internal medicine OPD and pulmonary medicine OPD). Patient’s complete medical history was collected by personal interview and other relevant information including detailed prescription was recorded in case record form.
Calculating prescription quality index scores using the prescription quality index tool
Hassan et al. [17] have rated drug indication and dosage as very important and given the highest weighted scale of ‘0’ to ‘4’. Fifteen criteria namely evidence-base, effectiveness, correct directions, practical directions, drug–drug interactions, drug–disease interactions, adverse drug reaction, duration, compliance, legibility, prescriber’s information, patient’s information, medication’s name, diagnosis, and patient’s improvement were considered as important and assigned the medium score of ‘0’ to ‘2’. Five criteria including unnecessary duplication, cost, generic prescribing, formulary or essential drug list, and requirement for drug therapy were rated as least important and assigned the lowest score of ‘0’ to ‘1’. Thus, each criterion carried a specific maximum score depending on its importance. [17]
As described in PQI, if the prescription consisted of more than one drugs, each drug was rated individually. Similarly, if patients suffered from more than one disease states, each disease state was rated separately. The minimum score was then selected for the PQI summation. If a drug was not indicated, criterion 1 was scored as ‘0’. Subsequently, criterion 2 (dosage), criterion 13 (duration) and criterion 14 (cost minimization) were all scored as ‘0’. The PQI total score was obtained by summing up all the minimum scores for the 22 criteria for all drugs in a prescription. The possible maximum score of the PQI was ‘43’. Prescription with the PQI total score of ≤31 was interpreted as poor quality, score 32–33 as medium quality and score 34–43 as high quality as described in PQI tool. [17]
To evaluate different items in the questionnaire standard references or publications were used. The primary references were PQI manual, pharmacy/pharmacology texts, credible medical journals or established websites. Examples are A to Z drug facts, [18] USPDI, Evidence Based Medical Reviews, Martindale’s Complete Drug Reference, [19] WHO essential drug list 2011, [20] National list of Essential medicines of India 2011, [21] National Formulary of India 2011 [22] British National Formulary (BNF) 2011 [23] and articles on Medline and Pub MED. For the cost of the therapy current issues of commercial sources like Current Index of Medical Specialities, [24] Monthly Index of Medical Specialties [25] and Indian Drug Review [26] were reviewed.
Statistical analyses
Data were analyzed using Statistical Package for Social Science version 20 manufactured by SPSS Inc. Descriptive statistics were used to describe the samples. Mean and standard deviation were used to describe numerical variables. Frequency (%) was used for categorical variables. To check the normality of data Shapiro–Wilk test was applied. Nonparametric tests were applied due to skewed distribution of the data. To validate the PQI internal consistency was measured using item total correlation and Cronbach’s α. These two properties reflect the extent to which items correlate with the total score and how well items measure the same construct. Correlation of criteria should be between 0.2 and 0.8 [17] Floor effects (percentage of prescriptions with minimum possible score) and ceiling effects (percentage of prescriptions with maximum possible score) were also assessed. Factor analysis [27] was performed to explore common dimensions between the PQI criteria. P <0.05 was considered significant.
Results
Characteristics of the patients with hypertension
A total of 222 patients received 222 prescriptions with 1063 drugs. Mean age of patients was 56 ± 15.1 (range 4–87 years) with 51.8% male patients. The number of drugs in the prescriptions ranged from one to ten with the mean value of 4.8 ± 2. The mean number of medical illnesses was 1.3 ± 1.1.
Total 122 (54.9%) prescriptions of hypertension and 100 (45%) of asthma patients were collected from internal medicine and pulmonary medicine OPD respectively [Table 1].
| Parameters | Tertiary health care facility (n (%)) | Total (n=222) | ||
|---|---|---|---|---|
| Medicine department hypertension (122) |
Pulmonary medicine bronchial asthma (100) |
|||
| Age group (year) | ||||
| ≥65 | 41 (33.60) | 27 (27) | 68 (30.6) | |
| <65 | 81 (66.39) | 73 (73) | 154 (69.4) | |
| Gender | ||||
| Male | 64 (52.46) | 51 (51) | 115 (51.8) | |
| Female | 58 (47.54) | 49 (49) | 107 (48.2) | |
| Number of diseases/ | ||||
| condition per prescription | ||||
| 1 disease/condition | 37 (30.3) | 73 (73) | 110 (49.5) | |
| 2 diseases/conditions | 57 (46.7) | 19 (19) | 76 (34.2) | |
| 3 diseases/conditions | 21 (17.2) | 7 (7) | 28 (12.6) | |
| 4 diseases/conditions | 6 (4.9) | 1 (1) | 7 (3.2) | |
| 5 diseases/conditions | 1 (0.8) | 0 | 1 (0.5) | |
| 6 diseases/conditions | 0 | 0 | 0 | |
| Number of drugs in the | ||||
| prescriptions | ||||
| 1 drug | 6 (4.9) | 6 (6) | 12 (5.4) | |
| 2 drugs | 13 (10.7) | 7 (7) | 20 (9.1) | |
| 3 drugs | 13 (10.7) | 16 (16) | 29 (13.1) | |
| 4 drugs | 28 (22.9) | 12 (12) | 40 (18) | |
| 5 drugs | 23 (18.9) | 19 (19) | 42 (18.9) | |
| 6 drugs | 15 (12.3) | 13 (13) | 28 (12.6) | |
| 7 drugs | 11 (9) | 18 (18) | 29 (13.1) | |
| 8 drugs | 11 (9) | 5 (5) | 16 (7.2) | |
| 9 drugs | 1 (0.8) | 4 (4) | 5 (2.3) | |
| ≥10 drugs | 1 (0.8) | 0 | 1 (0.5) | |
Table 1: Demographical and clinical features of patients at tertiary health care facilities (n=222)
The Prescription Quality Index
The PQI could be evaluated in about 15–20 min, depending on the number of drugs in the prescription.
Psychometric properties of the prescription quality index
The mean PQI total score was 32.1 ± 5.1. There was no significant difference in mean PQI score between hypertension - mean score 31.6 ± 5.6 and bronchial asthma-mean score 32.8 ± 4.3. The PQI score can range from 0 to 43. There was one (0.45%) prescription with a minimum score of 15, whereas 1 (0.45%) prescription scored maximum 40, indicating the absence of floor and ceiling effects. The total PQI scores were not normally distributed.
Table 2 shows the PQI mean scores for each PQI criterion. As criterion 18, prescriber’s information was a constant value; it was neglected in the analysis. None of the 22 criteria was normally distributed. All showed a skewed distribution as verified by using Shapiro–Wilk test.
| Criterion | Maximum score | Score (mean±SD) |
|---|---|---|
| Is there an indication for the drug? | 4 | 3±1.3 |
| Is the dosage correct? | 4 | 3.5±1.2 |
| Is the medication effective for the condition? | 2 | 1.5±0.7 |
| Is the usage of the drug for the indication | 2 | 1.4±0.6 |
| supported by evidence? | ||
| Are the directions for administration correct? | 2 | 1.8±0.4 |
| Are the directions for administration | 2 | 1.8±0.4 |
| practical? | ||
| Are there clinically significant drug‑drug | 2 | 1.6±0.5 |
| interactions? | ||
| Are there clinically significant drug‑disease/ | 2 | 1.8±0.5 |
| condition interactions? | ||
| Does the patient experience any adverse | 2 | 1.5±0.5 |
| drug reaction (s)? | ||
| Is there unnecessary duplication with other | 1 | 1.1±0.8 |
| drug (s)? | ||
| Is the duration of therapy acceptable? | 2 | 1.6±0.8 |
| Is this drug the cheapest compared to other | 1 | 0.1±0.2 |
| alternatives for the same indication? | ||
| Is the medication being prescribed by generic | 1 | 0.3±0.5 |
| name? | ||
| Is the medication available in the formulary | 1 | 1.0±0.8 |
| or essential drug list? | ||
| Does the patient comply with the drug | 2 | 1.4±0.8 |
| treatment? | ||
| Is the medication’s name on the prescription | 2 | 1.6±0.5 |
| clearly written? | ||
| Is the prescriber’s name on the prescription | 2 | 1.9±0.2 |
| legible? | ||
| Is the prescriber’s information on the | 2 | 1.6±0.5 |
| prescription adequate? | ||
| Is the patient’s information on the | 2 | 1.2±0.5 |
| prescription adequate? | ||
| Is the diagnosis on the prescription clearly | 2 | 1.0±0.5 |
| written? | ||
| Does the prescription fulfil the patient’s | 1 | 1.1±0.5 |
| requirement for drug therapy? | ||
| Has the patient’s condition (s) improved with | 2 | 1.3±0.6 |
| treatment? | ||
| Total score | 43 | 32.1±5.1 |
SD: Standard deviation, PQI: Prescription quality index
Table 2: Criteria wise mean PQI scores (n=222)
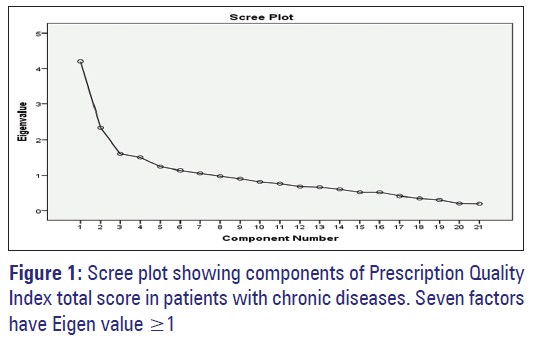
Exploratory principal components analysis of the PQI total scores revealed a seven-factor solution using the minimum Eigenvalue criteria of ≥1. These seven accounted for 62.4% of the total variance [Figure 1]. Cronbach’s α for the entire 22 criteria was 0.71.
The total PQI score was negatively correlated with age (correlation coefficient r = −0.057, P = 1) and number of drugs in the prescriptions (correlation coefficient r = −0.209**, P = 0.115). It showed no correlation with number of chronic diseases/conditions ([correlation coefficient r = 0.006**, P = 0.350]. **Correlation is significant at the 0.01 level [2-tailed]).
Out of 22 PQI criteria, PQI total scores were strongly correlated with drug indication and drug effectiveness, the evidence base, correct directions, unnecessary duplication and duration of therapy. There was weak to moderate correlation between the PQI total scores and the remaining criteria [Table 3].
| Criteria number | PQI criterion | Correlation with PQI total score (n=222) | |
|---|---|---|---|
| Correlation coefficient | P | ||
| 1 | Indication | 0.768** | <0.001 |
| 2 | Dosage | 0.559** | <0.001 |
| 3 | Effectiveness | 0.705** | <0.001 |
| 4 | Evidence‑based | 0.688** | <0.001 |
| 5 | Correct directions | 0.267** | <0.001 |
| 6 | Practical directions | 0.245** | <0.001 |
| 7 | Drug-drug interactions | 0.292** | <0.001 |
| 8 | Drug-disease/condition interactions | 0.201** | 0.003 |
| 9 | Adverse drug reaction | 0.200** | 0.003 |
| 10 | Unnecessary duplication | 0.612** | <0.001 |
| 11 | Duration of therapy | 0.627** | <0.001 |
| 12 | Cost | 0.274** | <0.001 |
| 13 | Generic prescribing | 0.166* | 0.013 |
| 14 | Formulary or essential drug list | 0.207** | 0.002 |
| 15 | Compliance | 0.207** | 0.002 |
| 16 | Medication’s name | 0.174** | 0.009 |
| 17 | Legibility | 0.018 | 0.793 |
| 18 | Prescriber’s information | 1 | ‑ |
| 19 | Patient’s information | 0.156* | 0.020 |
| 20 | Diagnosis | 0.086 | 0.202 |
| 21 | Requirement for drug therapy | 0.306** | <0.001 |
| 22 | Patient’s improvement | 0.369** | <0.001 |
**Correlation significant at 0.05 level (two‑tailed), *Correlation significant at 0.01 level (two‑tailed) spearman’s correlation. PQI: Prescription quality index
Table 3: PQI total score correlation with 22 criteria
Table 4 depicts the PQI score and quality of prescribing. Out of 222 prescriptions 80 (36%) were of poor quality. The proportion of total high and poor quality of prescription did not differ significantly (Chi-square test, P = 0.2029). There was no significant difference in proportion of high (P = 0.6080), medium (P = 0.1633) and poor (P = 0.6660) quality prescriptions between hypertension and bronchial asthma.
| Quality | PQI score | Tertiary health care facility (%) | Total (n=222) (%) | Chi ‑ square (P) | |
|---|---|---|---|---|---|
| Medicine department hypertension (n=122) | Pulmonary medicine bronchial asthma (n=100) | ||||
| Poor | ≤31 | 46 (37.7)* | 34 (34)* | 80 (36)# | 0.1863 (0.6660)* |
| Medium | 32-33 | 17 (13.9)** | 22 (22)** | 39 (17.6) | 1.943 (0.1633)** |
| High | 34-43 | 59 (48.4)*** | 44 (44)*** | 103 (46.4)# | 0.2631 (0.6080)*** |
Chi‑square test, #P=0.2029, for comparison between proportion of total poor quality prescriptions and high quality prescriptions. *Proportion of poor quality of prescriptions equal at both OPDs, **Proportion of medium quality of prescriptions equal at both OPDs, ***Proportion of high quality of prescriptions equal at both OPDs. OPDs: Outpatient departments, PQI: Prescription quality index
Table 4: PQI score and quality of prescribing
Discussion
This study was planned to evaluate the quality of prescribing for two chronic conditions, hypertension and asthma, in outpatient setting of a THC facility in western part of India with the help of PQI tool developed by Hassan et al. in 2010. [17] The PQI tool is already validated and claimed to be reliable and hence it was selected for assessment of prescribing quality.
The PQI total scores and individual criterion scores were not normally distributed. Hassan et al. [17] reported that two criteria (generic prescribing and diagnosis) were normally distributed, while the other criteria displayed skewed distribution. Only one (0.45%) prescription received a minimum score of 15, and one (0.45%) prescription received a maximal score of 40, indicating the absence of floor and ceiling effects. This finding is consistent with the previous study. [17]
Often instruments that have been tested in the same population might not need further testing, but further psychometric testing is necessary if differences exist between the study population and the population sampled when the instrument was developed and tested. Psychometric properties of tools used in the current study are necessary to report because they are specific to the sample of participants. [28] In our study exploratory principal components analysis of the PQI total scores exposed a seven-factor solution using the minimum Eigenvalue criteria of ≥1. These seven factors accounted for 62.4% of the total variance. Hassan et al. [17] reported an eightfactor solution using the minimum Eigenvalue criteria of ≥1. These eight factors accounted for 66% of the total variance. The value of Cronbach’s α for the entire 22 criteria was 0.71 compared with 0.60 in the previous study [17] suggesting that the PQI tool is valid and reliable in our setting also. Exploratory factor analysis of the PQI identified the multiple factors contributing to prescription quality.
There was no significant difference in prescribing quality in terms of PQI score between hypertension and bronchial asthma prescriptions (P > 0.05). For both the conditions, the quality of prescribing is better than at primary and secondary health care facilities with approximately 46.4% prescriptions with PQI score ranging from 34 to 43 compared to only 26% at later facilities. [29] There could be certain factors that may affect the quality of prescribing like; patients’ illness status including co morbidities, number of drugs prescribed and patients flow at health care center. Around 66% of prescriptions scored as medium to high for bronchial asthma at pulmonary medicine OPD compared to 62.3% for hypertension at internal medicine department. We have conducted a study at a tertiary care teaching hospital where prescriptions are written by consultant physicians as well as post graduate students. Hence, it would be possible to modify the prescribing quality by communicating the results to them. One of the important factors is practice of electronic prescribing (E-prescribing) at pulmonary medicine OPD which may influence the quality of prescribing. Health information technology, particularly E-prescribing, is a potentially powerful tool for improving safety. [30] At THC majority of patients have multiple problems with complications. Moreover at THC varied numbers of brand and/or essential drugs are available compared to primary health care (PHC) and secondary health care (SHC). Furthermore, larger numbers of physicians (prescribers) are available at THC as compared to PHC SHC. Several studies have demonstrated that the frequency of unnecessary or nonrecommended medication use is higher in patients taking many medications than in those taking few medications [31,32] as polypharmacy is more frequent at THC facility which can increase chances of irrationalities. There was an inverse correlation between the number of drugs prescribed and quality of prescribing. The higher the number of drugs prescribed in a prescription, the lower the prescription quality. This finding is consistent with the study by Hassan et al. [17] In a review of studies on polypharmacy and inappropriate drug use among older people, the frequency of inappropriate drug use was higher in study groups with polypharmacy (≥5 drugs), being 27–56%, compared to groups without polypharmacy (<5 drugs), for which the prevalence of inappropriate drug use was 10–23%. [33,34] Our study demonstrated a negative correlation of PQI total score with age and a lack of correlation with a number of diseases/conditions which was also reported by Hassan et al. [17] This finding could be due to the fact that at THC patients with moderate to severe illness are treated and varied ranges of drugs are prescribed which are available as per the hospital formulary and policy. Moreover sizable fraction of patients with the two diseases attending the facilities were above 50 years of age and hence complex prescribing led to poorer quality of prescribing and reduced PQI score.
The PQI total scores were strongly correlated with drug indication and drug effectiveness. There was moderate to weak correlation for reaming criteria. In a study by Hassan et al. the PQI total scores were strongly correlated with drug indication and drug dosage. There was moderate (six criteria) to weak (10 criteria) correlation and no correlation between the PQI total scores and four criteria namely unnecessary duplication, formulary/essential drug, legibility, and adequate patient information. However they were retained in PQI. [17] Our study shows at least one of these-unnecessary duplication moderately correlated with PQI total score suggesting regional variation in the factors affecting PQI score and prescription quality. As expected, drug indication shows a strong correlation with total PQI score and can have a major impact on quality of prescribing. These findings are consistent with the previous study at primary and secondary health care settings in India. [29]
Hassan et al. developed and validated PQI retrospectively that may have retrospective bias. In this study, data were collected prospectively for a fixed period with the advantages of completeness of data and proper sampling. We selected only two chronic conditions so as to minimize disease/condition variation which is reflected in better internal consistency in form of higher value of Cronbach’s α. as compared to the previous study. [17] Sample size is statistically sufficient at 80% power to derive a conclusion. To the best of our knowledge, no other study has used PQI tool for assessment of quality of prescribing in THC settings. Use of data from only one healthcare facility can be a limitation of the study. However as it was necessary to validate the tool in Indian setup one center was selected to begin with.
Our study suggests that PQI is a reliable tool for assessing prescribing quality and further studies in different health care settings and in conditions other than hypertension and bronchial asthma can be carried out using PQI for assessment of prescribing quality in differing therapeutic situations.
Conclusion
Based on our findings of prescription quality using PQI tool, about half of prescriptions for hypertension and bronchial asthma at the tertiary care hospital selected for our study are of good quality. PQI is a valid and reliable tool for measuring prescription quality in Indian health care setup and can be useful for observational as well as interventional studies.
Acknowledgments
We would like to thank Dr. Norul Badriah Hassan, Department of Pharmacology, School of Medical Sciences, Universiti Sains Malaysia, for providing PQI manual and guidance. We would also like to thank Dr. Utpala Kharod Dean of Pramukhswami Medical College and Physicians of Shree Krishna Hospital at Karamsad for permission to collect data and cooperation.
References
- Steinman MA, Landefeld CS, Rosenthal GE, Berthenthal D, Sen S, Kaboli PJ. Polypharmacy and prescribing quality in older people. J Am Geriatr Soc 2006;54:1516-23.
- Rochon PA, Gurwitz JH. Prescribing for seniors: Neither too much nor too little. JAMA 1999;282:113-5.
- Andersen M. Is it possible to measure prescribing quality using only prescription data? Basic Clin Pharmacol Toxicol 2006;98:314-9.
- Herbert CP, Wright JM, Maclure M, Wakefield J, Dormuth C, Brett- MacLean P, et al. Better prescribing project: A randomized controlled trial of the impact of case-based educational modules and personal prescribing feedback on prescribing for hypertension in primary care. Fam Pract 2004;21:575-81.
- Søndergaard J, Andersen M, Støvring H, Kragstrup J. Mailed prescriber feedback in addition to a clinical guideline has no impact: A randomised, controlled trial. Scand J Prim Health Care 2003;21:47-51.
- Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med 1997;157:1531-6.
- Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: Results of a US consensus panel of experts. Arch Intern Med 2003;163:2716-24.
- Hanlon JT, Schmader KE, Samsa GP, Weinberger M, Uttech KM, Lewis IK, et al. A method for assessing drug therapy appropriateness. J Clin Epidemiol 1992;45:1045-51.
- Desalegn AA. Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, south Ethiopia: A cross-sectional study. BMC Health Serv Res 2013;13:170.
- Ruths S, Straand J, Nygaard HA. Multidisciplinary medication review in nursing home residents: What are the most significant drug-related problems? The Bergen District Nursing Home (BEDNURS) study. Qual Saf Health Care 2003;12:176-80.
- Socialstyrelsen [Swedish National Board of Health and Welfare]. Indicators for Evaluation of the Quality of Drug Therapy Among Elderly REPORT; 2003. p. 110-20.
- Ni K, Siang C, Ramli M. Noncompliance with prescription writing requirements and prescribing errors in an outpatient department. Malays J Pharm 2002;1:45-50.
- Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med 1991;151:1825-32.
- Hennessy S, Bilker WB, Zhou L, Weber AL, Brensinger C, Wang Y, et al. Retrospective drug utilization review, prescribing errors, and clinical outcomes. JAMA 2003;290:1494-9.
- Lagerløv P, Hjortdahl P, Saxegaard L, Andrew M, Matheson I. Structuring prescribing data into traffic-light categories; a tool for evaluating treatment quality in primary care. Fam Pract 2001;18:528-33.
- Coste J, Venot A. An epidemiologic approach to drug prescribing quality assessment: A study in primary care practice in France. Med Care 1999;37:1294-307.
- Hassan NB, Ismail HC, Naing L, Conroy RM, Abdul Rahman AR. Development and validation of a new Prescription Quality Index. Br J Clin Pharmacol 2010;70:500-13.
- Tatro DS. A to Z Drug Facts. 5th ed. St. Louis, MO: Wolters Kluwer Health Inc.; 2004.
- Sweetman SC. Martindale: The Complete Drug Reference. 34th ed. London, UK: Pharmaceutical Press; 2011.
- WHO Model List of Essential Medicines. Available from: http://www. who.int/medicines/publications/essentialmedicines/en/index.html. [Last cited on 2011 Jun 24].
- National List of Essential Medicines of India. New Delhi: Government of India, Ministry of Health and Family Welfare; 2011.
- National Formulary of India. 4th ed. India: Government of India, Ministry of Health and Family Welfare, Indian Pharmacopoeia Commission; 2010.
- British National Formulary (BNF). London: Pharmaceutical Press; 2011.
- Current Index of Medical Specialities. India: UBM Medica India Private Limited; 2011.
- Gulhati CM, editor. Monthly Index of Medical Specialities. India: Indraprastha Press; 2011.
- Indian Drug Review. India: UBM Medica India Private Limited; 2011.
- Skyggedal Rasmussen HM, Søndergaard J, Sokolowski I, Kampmann JP, Andersen M. Factor analysis improves the selection of prescribing indicators. Eur J Clin Pharmacol 2006;62:953-8.
- DeVon HA, Block ME, Moyle-Wright P, Ernst DM, Hayden SJ, Lazzara DJ, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh 2007;39:155-64.
- Suthar JV, Patel VJ. Prescribing quality in patients with chronic diseases at primary and secondary health care facilities using prescription quality index tool. Int J Basic Clin Pharmacol 2014;3:553-9.
- Ammenwerth E, Schnell-Inderst P, Machan C, Siebert U. The effect of electronic prescribing on medication errors and adverse drug events: Asystematic review. J Am Med Inform Assoc 2008;15:585-600.
- Fialová D, Topinková E, Gambassi G, Finne-Soveri H, Jónsson PV, Carpenter I, et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA 2005;293:1348-58.
- Zhan C, Sangl J, Bierman AS, Miller MR, Friedman B, Wickizer SW, et al. Potentially inappropriate medication use in the community-dwelling elderly: Findings from the 1996 Medical Expenditure Panel Survey. JAMA 2001;286:2823-9.
- Bjerrum L, Søgaard J, Hallas J, Kragstrup J. Polypharmacy: Correlations with sex, age and drug regimen. A prescription database study. Eur J Clin Pharmacol 1998;54:197-202.
- Elmståhl S, Linder H. Polypharmacy and inappropriate drug use among older people – A systematic review. Healthy Aging Clin Care Elder 2013;5:1-8.