Prescribing Pattern for Skin Diseases in Dermatology OPD of in Boru Meda Hospital, North East, Ethiopia
Citation: Tegegne A. Prescribing Pattern for Skin Diseases in Dermatology OPD of in Boru Meda Hospital, North East, Ethiopia. J Basic Clin Pharma 2018;9:31-33.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Introduction: Skin diseases are the major contributors of disease burden in society. The ultimate goal in dermatological therapy is to use the safest and least number of drugs in order to obtain the best possible effect in the shortest period at reasonable cost. The problem gets compounded with the inappropriate and irrational use of medicines. Therefore, periodic prescription audit in the form of prescribing patterns is away to improve irrational prescription. The objective of this study to assess the prescription patterns of dermatological agents in Boru Meda hospital. Methods: Hospital based retrospective cross-sectional study in which prescribing patterns of dermatological agents are assessed. A total of 385 samples of patient record prescription from November/1/2016 to December/30/2016, and the sample were selected by systematic random sampling technique. Sample prescriptions were reviewed using structural data collection format. The Collected data was analyzed by using SPSS version 20. Results: Regarding sex and age of patients, the maximum numbers were male between the age group of 21-30 years (25.52%) and in female 21-30 years (32.64%). Topical steroids were the most commonly prescribed drugs (25.3%). The prevalence of atopic dermatitis was higher (26.3%, 20.8%) in both male and female respectively followed by scabies in male with 12.2% and Acne vulgaris (12.9%) in female. Number of drugs per prescription was higher (2.46) than WHO standard (<2). Conclusion: The current study reveals that topical corticosteroids were commonly prescribed drugs in the dermatology unit and the prescribing practice imitates incidence of polypharmacy.
Keywords
Boru Meda hospital; dermatological agents; prescription patternsIntroduction
Skin disease refers to disorders exclusively of the superficial layers of the skin. The commonest skin disorders seen in developing countries are psoriasis and scabies, but they have not been regarded as a significant problem that could benefit from public health measures. Most skin diseases are chronic and require lifetime treatment.[1] Improved quality of life by enhancing standards of medical treatment at all levels of the health care delivery system. Setting standards and assessing the quality of care through performance review should become part of everyday clinical practice.[2]
Prescribing patterns studies are useful to monitor evaluate and suggest modifications in prescribers, prescribing habits so as to make medical care rational and cost effective. Such analysis not only improves the standards of medical treatment at all levels in the health system, but also supports in the identification of drug use related problems such as, drug-drug interaction, poly-pharmacy and adverse drug reaction.[3,4] Irrational prescribing has a serious impact on health and economy, resulting in wastage of resource. The patterns of drug use in a hospital setting need to be monitored intermittently in order to analyze their rationality and increase the therapeutic benefits and reduce adverse effect.[5]
Methods
Study area and period
Boru Meda Hospital (BMH) is found in Eastern Amhara South Wollo zone, Dessie town, which is found about 411 km away from Addis Ababa, the capital city of Ethiopia. It was established in 1947 EC through the support of missionary organization that was primary focused on dermatology and ophthalmic services. It has a total of 80 beds among these 30 beds is in dermatological ward. The study was conducted from November 01/2016-December 30/2016.
Study design and study population
A retrospective institutional based quantitative cross sectional study was conducted by reviewing prescriptions and the sample were selected by systematic random sampling technique. The Study population of this study was all dermatological patients who were visit BMH, dermatology unit in outpatient department and for whom medicines were prescribed during study period.
Sampling technique and sample size
Sample size
The sample size for this particular study was calculated using formula for a single population proportion considering the following assumptions: A 95% confidence level, margin of error(0.05) and assume maximum variability (p=0.5). These parameters are substituted in the following single population proportion formula:
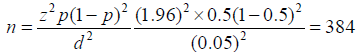
Where, n=Sample size; p=Proportion of people; d=margin of error (0.05); z=confidence level 95% (i.e., 1.96).
The population of annual dermatological patients at BMH is <10,000, therefore sample size adjustment is needed by using population correction formula:
(no=[ni/(1+(ni/N)])
Where, N=8400 (total number dermatological patients annually); ni=unadjusted sample size calculated. Sample size no=adjusted Sample size; no is equal to 367 and 5% for (incomplete information or data) makes the sample size 385.
Sampling technique
After sample size determined, Systematic random sampling technique was used to select the sample prescription.
Data collection and data analysis
Well-trained pharmacy personnel collected data on patient prescriptions. The specific types of data necessary to measure the prescription patterns were recorded for each patient prescription and entered directly into an ordinary prescription patterns form. After collection of the data, the data was entered in to SPSS version 20 for analysis.
Quality control
The data was verified by well-trained pharmacy personnel through direct supervision of principal investigators during the data Collection period.
Ethical consideration
The study was approved by chief executive officer, and the head of the pharmacy department in the BMH. A formal letter was written from BMH and given to pharmacy department and also confidentiality of the information obtained from the patient’s prescription reviewed throughout the study period was kept.
Results
The study includes a total of 385 patients and overall numbers of male patients were 192(49.9%) while numbers of female patients were 193(50.1%). The maximum numbers of patients were in male between the age group of 21-30 years (25.5%) and in female 21- 30 years (32.6%). The minimum numbers of patients were in male between Female >60 years (1.6%) [Tables 1-7].
| Age group | Male, n (%) | Female, n (%) |
|---|---|---|
| 0-10 | 31(16.2%) | 30(15.5%) |
| 11-20 | 47(24.5%) | 53(27.5%) |
| 21-30 | 49(25.5%) | 63(32.6%) |
| 31-40 | 19(9.9) | 22(11.4) |
| 41-50 | 20(10.4%) | 15(7.8%) |
| 51-60 | 14(7.3%) | 7(3.6%) |
| >60 | 12(6.3%) | 3(1.6%) |
| Total | 192 | 193 |
Table 1: Age with Sex distribution of the patients in dermatology unit of BMH (Dessie, 2016)
| Prescription item | Generic | Brand | Total |
|---|---|---|---|
| Single drug | 572(81.7%) | 128(18.3%) | 700 |
| Combination drug | 205(84.4%) | 38(15.6%) | 243 |
Table 2: Distribution of prescription item in Generic/Brand name in dermatology unit of BMH, 2016
| Route of administration | Number | Percentage (%) |
|---|---|---|
| Oral | 212 | 19.2% |
| Topical | 731 | 66.2% |
| Parentral | 1 | 0.1% |
| Combination(systemic& local) | 160 | 14.5% |
| Total | 1104 | 100% |
Table 3: Route of administration number of drugs prescribed in dermatology unit of BMH, 2016
| No. of drugs per prescription | No, of prescription, n (%) |
|---|---|
| 1 | 57(14.8%) |
| 2 | 180(46.8%) |
| 3 | 87(22.6%) |
| 4 | 42(10.9%) |
| 5 | 16(4.2%) |
| 6 | 1(0.3%) |
| 7 | 2(0.5%) |
| No. of drugs per prescription | 2.46 |
Table 4: No. of drugs per prescription in dermatology unit at BMH, Dessie, 2016
| Disease | Male, n(%)(467) | Female, n(%)(456) | Total |
|---|---|---|---|
| Atopic dermatitis | 123(26.3%) | 95(20.8%) | 218(47.1%) |
| Acne vulgaris | 34(7.3%) | 59(12.9%) | 93(20.2%) |
| Nummular eczema | 44(9.4%) | 48(10.5%) | 92(19.9%) |
| Sebohoric dermatitis | 31(6.6%) | 45(9.9%) | 76(16.5%) |
| Scabies | 57(12.2%) | 17(3.7%) | 74(15.9%) |
| Tinea captious | 24(5.1%) | 29(6.4%) | 53(11.5%) |
| Allergiccontact dermatitis | 14(3%) | 33(7.2%) | 47(10.2%) |
| Pityriasis alba | 23(4.9%) | 17(3.7%) | 40(8.6%) |
| Supper infected eczema | 22(4.7%) | 16(3.5%) | 38(8.2%) |
| Melasma | 11(2.4%) | 26(5.7%) | 37(8.1%) |
| Psoriasis | 13(2.8%) | 19(4.2%) | 32(7%) |
| Tinea pedis | 27(5.8%) | 4(0.9%) | 31(6.7%) |
| Viitiligo | 13(2.8%) | 16(3.5%) | 29(6.3%) |
| Cellulites | 18(3.9%) | 10(2.2%) | 28(6.1%) |
| Impetigo | 4(0.9%) | 17(3.7%) | 21(4.6%) |
| Onchomycosis | 9(1.9%) | 5(1.1%) | 14(3%) |
Table 5: Disease patterns in dermatology unit of BMH, 2016
| Drug category | No, of drug | Percentage |
|---|---|---|
| Topical steroid | 229 | 25.3% |
| Emollient* | 192 | 21.2% |
| Anti-biotic | 149 | 16.5% |
| Antifungal | 113 | 12.5% |
| Systemic steroid | 29 | 3.2% |
| Antihistamine | 24 | 2.7% |
| Vitamins | 3 | 0.3% |
| Anti-viral | 2 | 0.2% |
| Others** | 164 | 18.1% |
| Total | 905 | 100% |
*Emollient like: liquid paraffin, white petrolatum ointment, Neiva cream; **Others such as: salicylic acid powder, urea powder, metronidazole powder
Table 6: Category of drugs prescribed at the dermatology unit of BMH (Dessie, 2016)
| Parameters | No. of prescriptions on which specified | Percentage (%) |
|---|---|---|
| Frequency of application | 260 | 67.5 (%) |
| Duration of treatment | 216 | 56.1 (%) |
| Site of application | 208 | 54.0 (%) |
Table 7: Various parameters in the prescriptions of drug in dermatology unit of BMH, 2016
Most of topical steroids were prescribed by generic name. The number of drugs prescribed by brand name was 18.3% for drugs prescribed in single and 15.6% for drug prescribed in fixed dose combinations. Out of 1104 drugs, topical route 731(66.2%) was the most route of administration. oral route 212(19.2%) was the second most route of administration followed by a combination systemic and local route of administration.
Total number of drugs in 385 patients was found to be 946. Number of drugs per prescription varied from 1 to 7 with average of 3.0. Most of the prescriptions consists of minimum of 2 drugs (180 prescriptions, 46.75%). And the others with 14.80%, 22.60% contain a single drug and 3 drugs respectively.
Disease distribution
Out of 385 patients, prevalence of atopic dermatitis was higher in with (26.3%, 20.8%) both male and female respectively followed by scabies in male with 12.2% and Acne vulgaris (12.9%) in female by emollient (21.2%). Out of total of 905 The drugs prescribed, topical steroids were the most commonly used (25.3%), followed drugs 229 (25.3%) were Among topical drugs, Betamethasone cream/ointment was the most common prescribed drug. The most commonly prescribed drug was ketoconazole shampoo (50.9%) from the anti- fungal and doxycycline (37.7%) from anti-biotic. Out of 385 prescription drugs prescribed 67.5% frequency of application, 56.1% duration of treatment and 54.0% site of applications are specified. Consideration of various parameters while prescribing in the prescription of drugs.
Discussion
The results of this study provide valuable information on the prescribing patterns of doctors for dermatological patients at BMH. Many of the patients seen were in male between the age group of 21-30 years (25.5%) and in female 21-30 years (32.6%). This results were compare with in the past study done in Ayder referral hospital, which were maximum numbers of patients in male between the age group of 11-20 years (32.14%) and in female 11-20 years (31.63%). [6] Number of drugs per prescription varied from 1 to 7 with average of 2.46. Most of the prescriptions consists of minimum of 2 drugs (180 prescriptions, 46.8%). And the others with 14.8%, 22.6% contain a single drug and 3 drugs respectively. This study showed the incidence of polypharmacy. Polypharmacy is the use of an excessive number of inappropriate medicines. Average number of drugs per prescription reported in this study was very low as compared to studies by Sarkar et al. and Narwane et al. where average number of drugs prescribed were lesser than 3 drugs per prescription i.e., 2.7 and 2.64/prescription respectively.[7,8]
This study showed that atopic dermatitis (26.3%) and (20.8%) was the most common dermatological condition in the dermatology unit in both male and female respectively, Followed by scabies (12.2%) in male and acne vulgaris (12.9%) in female. different findings were also reported from study carried out in India the study showed fungal disease was the most common.[9] From the total of 1104 drugs prescribed, Topical corticosteroids were accounts for 731 (66.2%) followed by emollient (21.2%). This finding was similar with topical corticosteroids in Ayder referral hospital study and different from a study done by Bijoy et al. and Ashok et al. in India where Anti fungals were the most commonly prescribed.[9,10]
It is important that drugs should be prescribed in their generic names to avoid confusion and minimize the costs. But the result of the current study showed 18.3% of a single drug and 15.6% of drugs in fixed dose combinations were prescribed with brand name. This finding was different with the study done by ayder referral hospital study showed that 94.57% of a single drug and 100%of drugs in fixed dose combination were prescribed with brand name.[6]
The higher percentage of nonproprietary prescriptions in outpatients invokes the problem of the vast expenditure on such drugs and their availability in the hospital pharmacy. Many patients attending a hospital as out-patients belong to the lower socioeconomic status and would have to buy nonproprietary drugs from a low price. But he/she would have to buy proprietary drugs from high price and other relevant pharmacy outlets. Lack of trust in the quality of generic drugs could be the reason why brand names were highly prescribed. Among the total number of drugs prescribed, most of them were prescribed by topical (66.2%) followed by oral routes (19.2%) and the second most route of administration were a combination of systemic and local route of administration (14.5%). The reason for a high percentage of topical drugs being pre scribed is that topical route has minimum side effects hence is the preferred route of administration in dermatology. The use of fixed- Dose combinations may help to bring down the cost and improve compliance. According to Salwa Omer et al. study combination route of administration (systemic and local) was highly prescribed with a prevalence of 67.2% followed by oral route which was prescribed for 25.3% of cases.[11]
Frequency of application was specified only in 67.5% of prescriptions and duration of treatment and site of application was also steted in 56.1% and 54.0% of prescriptions respectively. This finding were similar with the study done by Ayder referral hospital, Ashok et al. and Sweileh.[6,9,12]
Conclusion
The current study reveals that average number of drugs per prescription was high (2.46) and topical corticosteroids were commonly prescribed drugs in the dermatology unit. This finding also showed that atopic dermatitis was the most prevalent disease condition.
REFERENCES
- World Health Organization. Epidemiology and Management of Common Skin 2006.
- Diseases in Children in Developing Countries.
- Chester BG. Polypharmacy in elderly patients with diabetes. Diabetes Spectrum 2002;15:240-8.
- Michael JC, John T, Catherine H, Julie C, Victoria B, Rachid TA, et al. An audit of adverse drug reactions to aqueous cream in children with atopic eczema. The Pharmaceut J 2003;271: 747-8.
- Chester BG. Polypharmacy in elderly patients with diabetes. Diabetes Spectrum 2002; 15: 240-8.
- Hafta BM, Martha K, Minyahil AW. Prescribing pattern in Dermatology unit of Ayder Referral Hospital. World J Pharmaceut Res 2014;4:17.
- Manjusha S, Kaveri DL, Soumya P, Pawar AP. Prevalance of various skin disorders and prescribing pattern of antihistamines in tertiary care hospital, Pune. Int J Pharma Sci and Res 2014;5.
- Audit Commission: A prescription towards more rational prescribing in general practice. HMSO 1994.
- Ashok Kumar M, Noushad PP, Shailaja K, Jayasutha J, Rmasamy C. A study on drug prescribing pattern and use of cortico steroids in dermatological conditions at a tertiary care teaching hospital. Int J Pharmaceut Sci Rev and Res 2011;9:69-71.
- Bijoy KP. Drug prescribing and economic analysis for skin Diseases in dermatology OPD of an India tertiary care teaching hospital: A periodic Audit. Ind J Pharmacy Practice 2012; 5:28-33.
- Salwa OB, Gamila H, Mohamed A. Prescription Patterns of Antibiotics in Five Dermatologic Outpatient Clinics; a Cross Sectional Study from Yemen. J Pham Pract Community Med 2016;2:65-9.
- Sweileh WM. Audit of prescribing practices of topical corticosteroids in outpatient dermatology clinics in north Palestine. Eastern Mediterranean Health J 2014;12:161-3.

