Management of coronary artery disease in a Tertiary Care Hospital
- *Corresponding Author:
- Mr. Pranay Wal
Department of Pharmacy, Jodhpur National University, Rajasthan, India.
E-mail: pranaywal@gmail.com
Abstract
Aims: The objective of the study was to study the prescribing patterns of drugs used in the coronary artery disease (CAD) and to identify, which drug is mostly prescribed at that hospital. Settings and Design: This was a prospective observational survey including case series analysis of patients with CAD who met the inclusion criteria. It was conducted in the cardiology unit of multidisciplinary Tertiary Care Hospital in Kanpur. Materials and Methods: Data of patients who met the inclusion criteria was collected in specially designed case record forms. It was designed to include the patient data such as, demographics, risk factors, clinical and biochemical characteristics, procedures and investigations performed during the hospital stay, in-hospital and discharge drug therapy. Statistical Analysis Used: Descriptive statistics were performed for baseline characteristics, risk factors and medication use. All the analyses were performed using Statistical Package for Social Sciences version 16.0. Results: Subjects of age groups 65-74 (33.34%) were found to be more susceptible to CAD. In this study, we see that Aspirin, Clopidogrel and Statins were mostly prescribed in this hospital. Conclusions: In this study, Aspirin and Clopidogrel were mostly prescribed. According to 2009 focused updates of American College of Cardiology/American Heart Association (ACC/AHA) guidelines for the management of patients with ST-elevation Myocardial Infarction. So in this hospital prescription for CAD were according to the guideline.
http://www.environmentjournals.com/
http://www.eventsupporting.org/
http://www.escientificreviews.com/
http://www.openaccesspublications.com/
http://www.imedpub.org/
http://www.jpeerreview.com/
http://www.escientificres.com/
http://www.scholarlyjournals.org/
http://www.eclinicaljournals.com/
http://www.scischolarsjournal.com/
http://www.intlscholarsjournal.com/
http://www.scholarsresjournal.com/
http://www.sysrevpharma.org/
http://www.environjournal.com/
http://www.jpeerres.com/
http://www.managjournal.org/
http://www.emedicalhub.org/
http://www.biomedresj.org/
http://www.aaccongress.com/
http://www.eclinicalres.org/
http://www.scholarlymed.com/
http://www.eclinicalres.com/
http://www.theresearchpub.com/
http://www.imedpubscholars.com/
http://www.scholarcentral.org/
http://www.journalpublications.org/
http://www.scholarlypub.com/
http://www.imedpublishing.org/
http://www.emedsci.com/
http://www.longdomjournals.org/
http://www.longdomjournal.org/
http://www.emedicalcentral.com/
http://www.lexisjournal.com/
http://www.geneticjournals.com/
http://www.scitecjournals.com/
http://www.microbialjournals.org/
http://www.engjournals.org/
http://www.eneurologyjournals.com/
http://www.pulsusjournal.org/
http://www.biochemjournal.org/
http://www.epharmacentral.com/
http://www.eclinicalsci.com/
http://www.eclinicalcentral.com/
http://www.eclinmed.com/
http://www.jopenaccess.org/
http://www.peerreviewedjournals.com/
http://www.immunologyjournals.com/
http://www.neurologyjournals.org/
http://www.clinicalmedicaljournals.com/
http://www.molecularbiologyjournals.com/
http://www.geneticsjournals.com/
http://www.biochemistryjournals.org/
http://www.psychiatryjournals.org/
http://www.pharmajournals.org/
http://www.alliedresearch.org/
http://www.medicalres.org/
http://www.medicalresjournals.com/
http://www.alliedsciences.org/
http://www.pediatricsjournals.org/
http://www.oncologyinsights.org/
Keywords
Aspirin, Clopidogrel, coronary artery disease, prescription pattern study
Introduction
“Hritshoola” an equivalent of present day angina/coronary artery disease (CAD) was known to ancient physicians since 500 BC. [1] Concurrent with the explosive growth of CAD among Indian diaspora, it has been observed that there are a substantial number of cases where none of the conventional major coronary risk factors such as smoking, hypertension, and hypercholesterolemia are present even though the patient gets CAD at a comparatively young age. [2-4] CAD is a collective term given to symptomatic manifestations of reduced blood flow in narrowed coronary arteries (those which supply the heart muscles). It is the term used to describe coronary arteries that are affected by pathological process. Cardiovascular disease is estimated to be the leading cause of mortality world-wide; responsible for 1/3rd of all deaths. [5] Despite the recent decline in developed countries, both CAD mortality and prevalence of risk factors continue to rise rapidly in developing countries. Rapid socio-economic growth in developing countries is increasing exposure to risk factors for CADs, such as diabetes, dyslipidemia, hypertension and smoking. [6] A dramatic increase in the prevalence of CADs is predicted in the next 20 years in the Indian subcontinent, due to rapid changes in demography and life-style consequent to economic development. Increasing rate of CAD mortality and the projected rise in CAD mortality for 2020 in the developing world necessitates immediate prevention and control measures. [7] The risk of CADs in Indians is 3-4 times higher than White Americans, 6 times higher than Chinese, and 20 times higher than Japanese. [8] It is now well-known that CADs tend to occur earlier in life in Indians than in other ethnic groups. Various studies have also shown rising prevalence of CAD in India. [9] Despite scientific evidence that secondary prevention medical therapies reduce mortality in patients with established CAD, these therapies continue to be underutilized in patients receiving conventional care. In recent years, the wide availability of randomized clinical trials has facilitated the development of guidelines for evidence-based treatment in cardiology by specialist panels. Various international organizations have formulated recommendations and guidelines for the management of CADs. One of the most used guideline was the result of a task force organized by the American College of Cardiology and American Heart Association. [10] Studies have shown that evidence based medicines, with therapy according to guidelines does improve patient outcome. [11]
This study was conducted in a cardiac hospital in Kanpur where we studied about patients’ demography, risk factors CAD are caused due to various underlying diseases among which, hypertension, diabetes, and dyslipidemia followed by smoking and family history are most common. In our study, CAD was found to be more prevalent in the age group of 65- 74 And also we see that ST Segment Elevation Myocardial Infarction (STEMI) patients needed acute therapy were treated with Thrombolytics, heparin Low molecular weight heparin, Unfractioned heparin (LMWH,UFH), Antiplatelets (Aspirin, Clopidogrel and GP2b/3a/1), Antianginals, Betablocker (BB, Nitrates, Angiotensin convertingenzyme inhibitor, Calcium channel blocker ACEI, CCB) and lipid lowering agents (Statins, Fibrates, Niacin, Ezetimib) and in NSTEMI except thrombolytic all other drugs were given and we find that As pirin and Clopidogrel were mostly prescribed.
Materials and Methods
Study design and setting
The study was conducted in the Cardiology unit of multidisciplinary Tertiary Care Hospital in Kanpur. This was a prospective observational study including case series analysis of patients with CAD who met the inclusion criteria. Cases were identified prospectively for a given period of time (November 2011 to December 2012) in this study site. Ethical clearance was obtained from the Institutional Ethics Committee. The study group consisted of all patients admitted in the Cardiology Department of hospitals, and who met the Inclusion criteria, Patients admitted in cardiology units who are diagnosed to have CAD, patients of both sexes, irrespective of age, and patients who have admitted in other specialties, who are not diagnosed to have coronary artery disorders and who are pregnant were excluded from the study.
Measurements
The list of patients admitted every day under cardiology unit was collected from the Medical Records Department (MRD). Case records of each patient admitted under cardiology unit were reviewed to identify patients with CAD. Data of patients who met the inclusion criteria was collected in specially designed case record forms. Source of data were collected from patient case records, which includes, patient history notes, patient drug treatment charts, reports of diagnostic and interventional procedures, laboratory investigations report, progress sheets, discharge summary, daily admission list maintained by MRD. It was designed to include the patient data such as demographics, risk factors, clinical and biochemical characteristics, procedures and investigations performed during the hospital stay, in-hospital and discharge drug therapy etc.
Statistical analysis
Descriptive statistics were performed for baseline characteristics, risk factors, and medication use. Data were presented as percentages for categorical variables with group comparisons made using the Chi-square tests, or likelihood ratio. An association of baseline factors with medication use was examined for beta blockers, and Angiotensin converting enzyme (ACE) inhibitors were also compared using a Chisquare test. The variables considered were age group, gender, and history of diabetes, hypertension, heart failure, myocardial infarction and bronchial asthma. All the analyses were performed using the Statistical Package for Social Sciences version 16.0. A P value of < 0.05 was considered statistically significant.
Result
The data collected was evaluated for demography, and treatment pattern. During the study period, 120 patients were logged, of whom 55 were with acute coronary syndrome (ACS) and 65 with other CADs. Out of 55 ACS patients, 35 were ST segment elevated myocardial infraction and 20 Non ST segment elevated myocardial infraction/unstable angina. Patient included as other CADs were those patients with documented CAD who have admitted for evaluation and procedures.
Demography
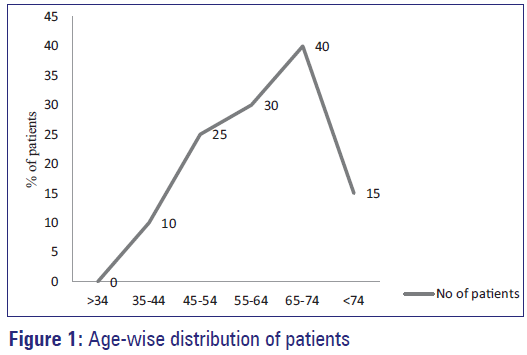
Age
The patients were divided in to six age groups ranging from > 34 years to < 74 years. Even though, CAD was found to be more prevalent in the age group of 65-74 and it is 33.34%. The age wise distribution of patients with CAD is summarized in Figure 1.
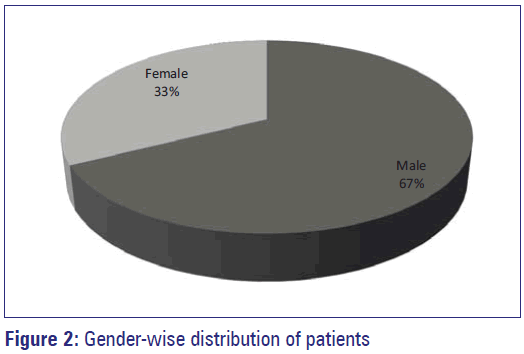
Gender
Gender wise distribution of patients with CAD is shown in Figure 2.
Diseases associated risk factors for CADs
A total of 120 patients with CAD were evaluated for the prevalence of risk factors. There were 81 (67%) male and 39 (33%) females in the study sample. Prevalence was represented as percentages and was calculated for male and female separately. Diabetes and Hypertension were more prevalent in women (64.10% and 92.30%) compared to men (43.21% and 49.38%) in this study. However, there was a higher prevalence of smoking in male (43.21%) than in female. The prevalence of risk factors for CAD was shown in Table 1.
| Risk factors | Male | Female | Over all |
|---|---|---|---|
| n=81 (67%) | n=39 (33%) | n=120 (%) | |
| Diabetes | 35 (43.21) | 25 (64.10) | 60 (50.00) |
| Hypertension | 40 (49.38) | 36 (92.30) | 76 (63.33) |
| Family history | 5 (6.17) | 10 (25.64) | 15 (12.50) |
| Smoking | 35 (43.21) | 0 | 35 (29.16) |
| Dyslipidemia | |||
| Total cholesterol>200 | 20 (24.69) | 10 (25.64) | 30 (25.00) |
| LDL>100 | 14 (17.28) | 10 (25.64) | 24 (20.00) |
| Triglycerides>150 | 7 (8.64) | 7 (17.95) | 14 (11.66) |
| HDL<40 | 9 (11.11) | 9 (23.07) | 18 (15.00) |
LDL: Low-density lipoprotein, HDL: High-density lipoprotein
Table 1: Risk factors for coronary artery diseases
Treatment pattern
Interventional procedures and drug therapy used were evaluated to study the treatment pattern.
Interventional procedures
Coronary Angiogram was performed in 80.55% of patients admitted with CAD. Percutaneous transluminal coronary angioplasty (PTCA) and Coronary artery bypass graft Surgery (CABG) were performed or scheduled in 38.88% and 17.59% of patients respectively.
Acute management
A total of 49 patients were evaluated for acute management of CAD, which included 29 STEMI and 20 UA/NSTEMI patients. In STEMI 29.58% of patients received thrombolytic therapy with streptokinase. Anticoagulation with LMWH was widely used both in STEMI (77.3%) and in NSTEMI/UA (70%). UFH was used only 13.79% and 5% of patients with STEMI and NSTEMI/UA respectively. All patients received Aspirin and Clopidogrel, except a few proportions in which Aspirin was contraindicated. Patients with UA/NSTEMI (45%) received platelet glycoprotein 3a/2b inhibitors more frequently compared to STEMI (29.28%) patients. Use of beta-blockers (79.31%, 85%) and ACE Inhibitors (62.05%, 75%) were widely accepted for the acute management of CAD in patients with STEMI and NSTEMI/UA. Lipid lowering therapy with statin was widely used both in STEMI (96.55%) and in NSTEMI/UA (100%). Use of niacin (0%), fibrates (3.44%) and ezetimibe (13.79%, 10%) were exceptional. Drug therapy given for the acute management of CAD is summarized in Table 2.
| Drug therapy | STEMI (%) | NSTEMI/UA (%) |
|---|---|---|
| n=29 | n=20 | |
| Thrombolytics | 8 (29.58) | - |
| Heparin | - | - |
| LMWH | 23 (79.31) | 14 (70) |
| UFH | 4 (13.79) | 1 (5) |
| Antiplatelets | ||
| Aspirin | 29 (100) | 20 (100) |
| Clopidogrel | 29 (100) | 19 (95) |
| GP11b/111a I | 8 (29.58) | 9 (45) |
| Antianginals | ||
| Beta blockers | 23 (79.31) | 17 (85) |
| Nitrates | 6 (20.68) | 7 (35) |
| ACEI | 18 (62.06) | 15 (75) |
| CCB | 2 (6.89) | 3 (15) |
| Lipid lowering drugs | ||
| Statins | 28 (96.55) | 20 (100) |
| Fibrates | 1 (3.44) | 0 |
| Niacin | 0 | 0 |
| Ezetimibe | 4 (13.79) | 2 (10) |
CA: Chronic angina, STEMI: ST elevated myocardial infraction, NSTEMI: Non ST elevated myocardial infraction, UA: Unstable angina, LMWH: Law molecular weight heparin, UFH: Un fractional heparin, ACEI: Angiotensin converting enzyme inhibitor, CCB: Calsium channel blocker
Table 2: Acute management of CA
Chronic management of CAD
Drug therapy given at discharge for all patients admitted with CAD was considered for chronic management. Total of 104 patients was evaluated for secondary prevention drug therapy. Antiplatelets Aspirin (98.07%) and Clopidogrel (98.07%) were widely used for chronic therapy. Among the antianginals with proven efficacy in the management of CAD, beta-blockers (69.33%) and ACE Inhibitors (66.34%) were prescribed frequently. All patients received lipid lowering therapy with statin. Use of fibrates (2.88%), niacin (7.69%) and ezetimibe (1.92%) were negligible. The drug therapy given for the chronic management of CAD were summarizes in Table 3.
| Drug therapy | No. of patients with CAD (n=104) |
|---|---|
| Antiplatelets | |
| Aspirin | 102 (98.07) |
| Clopidogrel | 102 (98.07) |
| Antianginals | |
| Beta blockers | 72 (69.23) |
| Nitrates | 24 (23.07) |
| ACEI | 69 (66.34) |
| CCB | 18 (17.30) |
| Lipid lowering drugs | |
| Statins | 100 (96.15%) |
| Fibrates | 1 (0.96) |
| Niacin | 0 |
| Eztimibe | 11 (10.57) |
CAD: Coronary artery disease, ACEI: Angiotensin converting enzyme inhibitors, CCB: Calciunm channel blocker
Table 3: Chronic management of CAD (secondary prevention)
Analysis of data
Data collected were evaluated for demography, risk factors and treatment pattern in the study site. The demographic data considered were age and gender. Treatments pattern both pharmacological and interventional therapies were evaluated. Pharmacological therapy include, drug therapy given for both acute (STEMI and NSTEMI/UA) and chronic (secondary prevention) management of CAD. The frequency of use of drug therapy was represented as percentages. The data regarding demography, risk factors and treatment pattern were studied at the hospital. Treatment pattern was compared to ACC/AHA guidelines.
Discussion
In this study, Aspirin and Clopidogrel were mostly prescribed. According to 2009 focused Updates of ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction, patients with definite or likely UA/ NSTEMI selected for an invasive approach should receive dual-antiplatelet therapy. Aspirin should be initiated on presentation and Clopidogrel is recommended as a second antiplatelet agent. In chronic therapy, Aspirin and Clopidogrel were only given as Antiplatelets and other treatment is same as acute therapy except thrombolytic and Heparin. Aspirin is an inexpensive and effective treatment for many patients with CAD. Although, clinical practice guidelines advocate the use of Aspirin for patients with ACS. [11,12] A similar study was conducted by (Masoudi et al. 2005) they said that Aspirin is an inexpensive and effective treatment for many patients with CAD. Marked variation in Aspirin prescription existed by state, with rates ranging from 31% to 70%. Patients with more severe CAD received Aspirin more frequently as part of their discharge regimen. Aspirin is an inexpensive and effective treatment for many patients with CAD. Although, clinical practice guidelines advocate the use of Aspirin for patients with ACS. [12,13] In another study, Aspirin prescription was positively correlated with ACE inhibitor treatment, implying that concerns about drug interactions did not entirely explain treatment decisions. Additionally, both the prescription of beta blockers and documentation of Left Venricular (LV) function-guideline recommended processes of care for patients with CAD and heart failure, respectively. [14,15]
Conclusion
In this study, the data collected was evaluated for demography and treatment pattern. Aspirin and Clopidogrel were mostly prescribed in this hospital and data were analyzed according to 2009 focused updates of ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction. We sure that this article will help the professionals for prescription.
References
- Sushruta Samhita, Commentator, Bhaskar G Ghanekar (Sheo Narain Upadhya). Naya Sansar, Vadini, Kashi, 1943.
- Gupta R, Gupta VP. Meta-analysis of coronary heart disease prevalence in India. Indian Heart J 1996;48:241-5.
- Krishna SS, Prasad NK, Jose VJ. A study of lipid levels in Indian patients with coronary artery disease. Int J Cardiol 1989;29:337-45.
- Bhatnagar D. The metabolic basis of increased coronary risk attributed to people from Indian subcontinent. Curr Sci 1998;74:1087-94.
- Ravi A, Rasalingam R, Thomas A. Pearson: An integrated approach to risk factor modification. In: Topol EJ, Calft RM, Isner JM, Prystowsky EN, Swain JL, Thomas JD, et al, editors. Text Book of Cardiovascular Medicine. 2nd ed., Vol. 2002. Lippincott Williams & Wilkins; 2008. p. 247-61.
- Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart J 2004;148:7-15.
- Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation 1998;97:596-601.
- Rissam HS, Kishore SN. Trehan coronary artery disease in young Indians - The missing link. J Indian Acad Clin Med 2001;3:128-32.
- Bhal VK, Prakashan D, Karthikeyan G. Coronary artery disease in Indians. Indian Heart J 2001.
- Fonarow GC, Gawlinski A, Moughrabi S, Tillisch JH. Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP). Am J Cardiol 2001;87:819-22.
- Kramer JM, Newby LK, Chang WC, Simes RJ, Van de Werf F, Granger CB, et al. International variation in the use of evidence-based medicines for acute coronary syndromes. Eur Heart J 2003;24:2133-41.
- Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, et al. 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol 1999;34:890-911.
- Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 2000;36:970-1062.
- Gibbons RJ, Chatterjee K, Daley J, Douglas JS, Fihn SD, Gardin JM, et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 1999;33:2092-197.
- Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: Executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 2001;38:2101-13.