Knowledge and Practice Regarding Dry Eye among General Population in Western Region of Saudi Arabia
Citation: Kalakattawi RM, Kalakattawi AM, Alsuqati FA et al. Risk of Obstructive Sleep Apnea (OSA) Assessment among Patients with Type 2 Diabetes in Taif, Saudi Arabia. J Basic Clin Pharma 2018;9:68-72.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Objective: Dry eye syndrome (DES) is a common disorder of the tear film caused by decreased tear production or increased evaporation and manifested with various signs and symptoms. This study aimed to assess the knowledge and practice regarding (DES) among population in western region of Saudi Arabia (KSA). Methodology: This study included 621 participants aged between 15 and 80 years from western KSA. Data collected using a self-administered questionnaire with multiple choice questions. Results: Results of our study showed that all of our participants suffering from (DES). No significant relation between age and gender were found. Most of Saudi adults watch TV or use a mobile phone or computer or any of smart hardware for long periods and daily or almost daily (86.5%), smoke cigarettes or shisha (59%). While about half of them do surgery to correct their eye (56%), and drive for long distances (49%). Also, results showed that about 34% reported pain or tingling in their eyes. About half of adults reported that they desire to itch their eyes (61%). Dryness of the eyes was complained by about 24% of participants. Burning sensation symptom was reported by 40.7% of participants. With regarding to the causes, dusty air (31%) and uses of electronic devices (25.4%) are the most reasons for dry eye symptoms reported by participant, followed by wearing contact lenses (15.9%). Conclusion: Results indicated that there is a high prevalence of (DES). Concerned must be increased about people knowledge regarding (DES) causes and symptoms.
Keywords
Dry eye syndrome; keratoconjunctivitis sicca; knowledge; Saudi Arabia
Introduction
Dry eye syndrome is a chronic, multifactorial disease. It is a tear film disorder due to increase tear evaporation or deficiency of tear which causes interpalpebral ocular surface damage and associated with ocular discomfort symptoms.[1] DES is also called keratoconjunctivitis sicca (KCS), keratitis sicca, sicca syndrome, xerophthalmia, dry eye disease (DED), ocular surface disease (OSD), or dysfunctional tear syndrome (DTS), or simply dry eyes.[2] discomfort symptoms and damage of the interpalpebral ocular surface are associated with Insufficient tears. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.[2] DES is associated with decreased ability to perform certain activities such as reading, driving, and computer related work, which require visual attention. Patients experience dry eyes symptoms constantly and severely, affecting their quality of life.[3]
Dry eye can be caused by deficiency of any one or more of the tear film component or can be a component of systemic diseases, including Sjogren’s syndrome, Lupus and Stevens Johnson’s Syndrome. Factors such as contact lens wear and adverse environmental exposures can exacerbate the symptoms of dry eye. Several studies showed the relationship of dry eye disease and the tear film, autoimmune mechanisms and skin diseases, while there is a recent study has identified further risk factors that include contact lens wear, eyelid and lacrimal gland damage and age.[4] On the other hand, there are various risk factors for dry eye which include air pollution, smoking, low humidity, high temperature, sunlight exposure and drugs.[5,6]
The main symptom of dry eyes is dry and gritty feeling in the eyes. Additionally, symptoms include burning or itching in the eyes, foreign body sensation, excess tearing, pain and redness of the eyes, and photophobia in some cases.[7] It is also associated with a stringy discharge and blurred, changing vision. Symptoms are found to worsen in dry weathers, with low humidity and higher temperatures.[8]
Since we all are exposed to such adverse conditions, dry eye affects nearly everyone at one time or another.[4] In addition, the prevalence of dry eyes varies from 10.8% to 57.1% and increases with age. DES is a common eyes disorder among the population, more affecting those older than 50 year old.[9] In contrast, the most commonly affected age group are the middle-age and older adults due to the high prevalence of refractive surgeries, systemic drug effects, autoimmune diseases and contact lens usage in these group.[10] Research also shows that DES can affect any race and is more common in women than in men. [11] In women at the age of 50–52 when menopause usually sets in, an imbalance occurs between the estrogen and androgen hormones This excites inflammation in lacrimal gland and ocular surface, disrupting the normal homeostatic maintenance of the lacrimal gland and ocular surface.[12]
Gupta et al. Conducted a study to estimate the prevalence of dry eye among 400 consecutive patients aged >40 years attending the ophthalmology outpatient department in hospital in India.[13] Schirmer’s tests, evaluations of tear-film breakup times and fluorescein staining of corneas were done. Results showed that the overall prevalence of dry eye was 29.25%, there was considerable age- and gender-related variation in this parameter. Compared with the younger patients, those aged = 80 years were more likely to have dry eye (41.2%), and the women investigated were more likely to have dry eye than the men (27% v.12%). According to this they concluded that dry eye syndrome is multifactorial disease and it’s associated to high prevalence.
Jamaliah and Fathilah studied the prevalence of dry eye in university Malaya Medical Centre.[14] Two hundred outpatients (115 females and 85 males) attending the University Malaya Medical Center (UMMC) eye clinic, aged 20 years and above and without any ocular surface disorder were recruited for the study. Their tear film status was determined subjectively by their symptoms and quantitatively by the cotton thread test, Schirmer’s test, marginal tear film meniscus assessment, fluorescein corneal staining and tear break-up time. The prevalence of dry eye in this sample population as defined by presence of symptoms and an abnormal test result is 14.5%. Presence of dry eye as detected by clinical testing is higher in the Chinese race (p< 0.01), in the group 40-59 years (p=0.024). There is no difference between females and males. Elderly patients have a lower Schirmer’s score.
Onwubiko et al. Determined the prevalence, distribution and risk factors for dry eye disease (DED) in a tertiary ophthalmic outpatient population.[15] The study was a cross-sectional descriptive hospital-based survey conducted at the Eye clinic of the University of Nigeria Teaching Hospital (UNTH). The participants comprised adult ophthalmic outpatients aged 18 years or older. Participants’ Sociodemgraphic data were obtained. Dry eye disease was assessed subjectively with the Ocular Surface Disease Index (OSDI) questionnaire; and objectively with Schirmer’s test and Tear-film Break-up Time (TBUT). An OSDI score of = 50 with a TBUT of < 10 s or Schirmer’s test reading of < 10 mm was considered diagnostic of DED. Descriptive and analytical statistics were performed. In all comparisons, a p< 0.05 was considered statistically significant. Results of the study showed that the prevalence of DED was 19.2%. Dry eye disease was significantly associated with age>40 years (OR 1.88, 95% CI 1.06-3.35, p=0.0004), non-possession of formal education (OR 0.40, 95% CI 0.21-0.74, p=0.001) but not gender (OR 1.48, 95% CI 0.89-2.46, p=0.158). They concluded that the prevalence of DED among ophthalmic outpatients at UNTH, Enugu, is comparatively high. Older age and illiteracy are predictors of DED. There is need for high index of diagnostic suspicion to prevent sightthreatening complications of DED.
Uchino et al. Investigated the tear function and prevalence of dry eye disease (DED) in visual display terminal (VDT) users.[16] Six hundred and seventy-two young and middle-aged Japanese office workers who used VDT completed questionnaires and underwent dry eye testing. The prevalence of DED was investigated using logistic regression analysis to examine associations between DED and possible risk factors. The risk factors, feature of ocular surface and prevalence of DED were evaluated. Results revealed that the percentage of women with a composite outcome of definite DED or probable DED was 76.5%, which was higher than that among men (60.2%). Workers over 30 years of age had a higher risk of DED (OR=2.22; 95% CI, 1.06-4.66), as did workers using a VDT >8 hours per day (OR=1.94; 95% CI, 1.22-3.09). Average Schirmer value was 18.7 ± 11.7 mm and tear break-up time (TBUT) was 4 ± 2.5 seconds (78.6% of study participants had TBUT = 5 seconds). These results concluded that DED is prevalent among young to middle-aged Japanese VDT users. Ophthalmic findings revealed short TBUT and corneal staining accompanied by normal Schirmer test values. Increased risk for DED was noted for women aged over 30 years and prolonged VDT use. Measures to modify the adverse impact of VDT use on the ocular surface may provide a positive impact on public health and quality of life for office workers using VDTs.
Xu et al. studied correlation between smoking and the incidence of dry eye.[17] Two cohort studies and eight cross-sectional surveys were included. Results indicated no statistically significant relationship between current (OR=1.32; 95% CI: 0.99-1.76; P=0.055) or ever smoking (OR=1.12; 95% CI: 0.98-1.28; P=0.107) and the risk of dry eye among the studies, even when age and gender were adjusted (OR=1.16; 95% CI: 0.83-1.64; P=0.383). In the sensitivity analysis in which only general population were included, the association was significant between smoking and dry eye (OR=1.50; 95% CI: 1.08-2.09; P=0.016). The conclusion of their results was the risk of dry eye may associate with smoking in general population.
The previous studies conducted to evaluate the prevalence of dry eye syndrome, its causes and symptoms at different regions. It was shown that dry eye syndrome is a multifactorial disease with high prevalence that must be in consideration. According to its relation to the environment condition and life habits and according to the lack of such like studies in Saudi Arabia, we conducted this study to evaluate the knowledge and practice of people toward this disease in western region of Saudi Arabia.
Methodology
A community based cross sectional study was conducted to assess the knowledge and practice regarding dry eye among general population in western region in Saudi Arabia. The oral consent to participate in the study was obtained from participants, after explanation of the study nature and their participation is voluntary. People from the general population are surveyed through a self-administrated face to face questionnaire over the period from March to May 2018, from different public areas such as hospitals, primary health care centers, universities, schools, shopping malls and gardens in overall western region in Saudi Arabia. The study involved 621 persons aged from 15-80 years and included both males and females. The research ethics committee in Taif University Taif, Saudi Arabia approved the research proposal of this study on 28 February 2018.
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 21.0, and applying the appropriate statistical tests. The continuous variable will be presented as mean ± SD and categorical variables will be presented as counts and percentages and the level of significance will be set at P = 0.05.
Results
This study included 621 participants aged between 15 and 80 years. Socio-demographic characteristics of the participants are presented in Table 1. Most of study sample were female. About half the participants aged 25 or less year age. 56% of the participants were from Taif city. Moreover, majority of participants were living in cities [Table 1].
| Variable | n (%) |
|---|---|
| Gender | |
| Male | 103 (16.6) |
| Female | 518 (83.4) |
| Age | |
| =25 | 359 (57.8) |
| 26-35 | 101 (16.3) |
| 36-45 | 91 (14.7) |
| 45> | 67 (10.8) |
| Residency | |
| Taif | 352 (56.7) |
| Makkah | 90 (14.5) |
| Jaddeh | 103 (16.6) |
| Almadinh | 30 (4.8) |
| Other | 45 (7.2) |
| Region | |
| City | 592 (95.3) |
| Village | 29 (4.7) |
| Medications | |
| Anti-allergy (pills or eye drops) | 77 (12.4) |
| Diuretics | 3 (0.5) |
| Pills to help you sleep | 6 (1) |
| Contraceptives | 36 (5.8) |
| Medicines for stomach ulcers | 10 (1.6) |
| Medicines for blood pressure | 17 (2.7) |
| Other | 26 (4.2) |
| Do not use drugs | 446 (71.8) |
Table 1: Socio-demographic characteristic of Saudi adults (n=621)
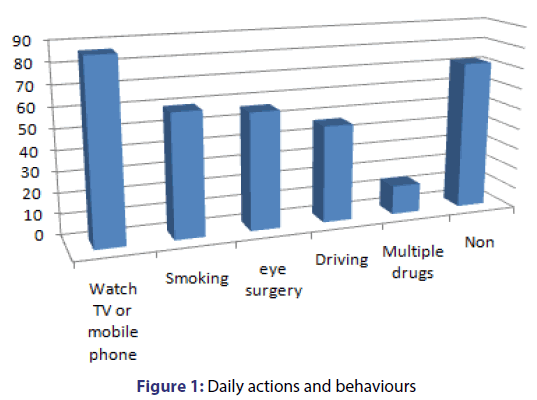
Furthermore, Figure 1 shows daily actions or behaviours among Saudi adults. Most of the study sample watch TV or use a mobile phone or computer or any of smart hardware for long periods and daily or almost daily (86.5%). While about half of them smoke cigarettes or Shisha (59%). Do surgery to correct their eye (56%), and drive for long distances (49%). Most of the study sample didn’t use any medication (71.8%) [Figure 1].
As presented in Table 2, 73.4% of participants did not wear any lenses. About half of them didn’t use any eye drop or drug for eye dryness.
| Variable | n (%) |
|---|---|
| Wearing lenses | |
| Soft lenses | 158 (25.4) |
| Solid lenses | 7 (1.1) |
| Non | 456 (73.4) |
| Receiving eye drop or drug for dryness | |
| Yes | 260 (41.9) |
| No | 297 (47.8) |
| didn’t remember | 64 (10.3) |
Table 2: Participants’ characteristics related to eyes
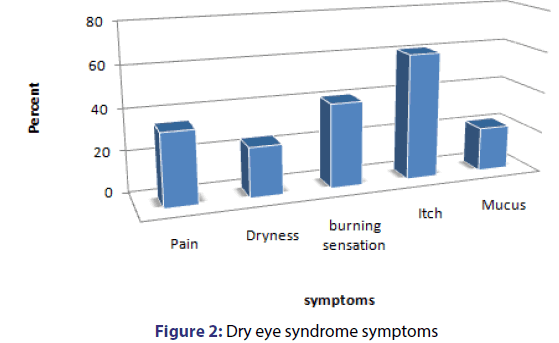
About 21% reported that they had mucus in the form of filaments around the eye or inside it and about 34% reported pain or tingling in their eyes. More than half of adults reported that they desire to itch their eyes (61%). Dryness of the eyes was complained by about 24% of participants. Burning sensation symptom was reported by 40.7% of participants, data presented in Figure 2.
As presented in Table 3, more than half of adults didn’t visit an eye doctor when they suffer any of dry eye symptom (58.8%). 51.9% of the participants use moisturizing eye drops to treat the symptoms. Only 9.3% of the adult suffer continuously from the symptoms. One third of the study sample reported that optometrist describe dry eye treatment for them the treatment (32.5%).
| Variable | n (%) |
|---|---|
| Visiting an eye doctor | |
| Yes | 258 (41.5) |
| No | 363 (58.5) |
| Frequency | |
| Rare | 216 (34.8) |
| Sometime | 236 (38) |
| Often | 111 (17.9) |
| Continuously | 58 (9.3) |
| Treating | |
| Moisturizing eye drops | 322 (51.9) |
| Nothing | 278 (44.8) |
| Other | 21 (3.4) |
| Describe the treatment | |
| Optometrist | 202 (32.5) |
| Pharmacist | 65 (10.5) |
| Friend | 34 (6.9) |
| Information from the Internet | 21 (3.4) |
| Other | 12 (1.9) |
| Didn’t use | 278 (44.8) |
Table 3: Some information about dry eye syndrome symptoms
The causes of dry eye symptoms are presented in Figure 3. Dusty air (31%) and uses of electronic devices (25.4%) are the most reasons for dry eye symptoms reported by participant, followed by wearing contact lenses (15.9%). On the other hand, exposed to sun, fumes or perfumes were one of the least reasons that cause dry eye symptoms according to the opinion of the participants.
Table 4 shows the general characteristics of participants. The majority of the participants hadn’t have arthritis or thyroid problems. Half of the participants hadn’t have also dryness in the nose or throat or mouth. Only 9.5% of the participants sleep with partially closed eye and 15% had trachoma.
| Variable | n (%) |
|---|---|
| Arthritis | |
| Yes | 116 (18.7) |
| No | 505 (81.3) |
| Thyroid problems | |
| Yes | 57 (9.2) |
| No | 564 (90.8) |
| Red eye and irritated when swimming | |
| Yes | 149 (24) |
| No | 243 (39.1) |
| Sometime | 229 (36.9) |
| Dryness in the nose or throat or mouth | |
| Yes | 76 (12.2) |
| No | 335 (53.9) |
| Sometime | 210 (33.8) |
| Sleep with partially closed eye | |
| Yes | 59 (9.5) |
| No | 439 (70.7) |
| Didn’t know | 123 (19.8) |
| Trachoma | |
| Yes | 93 (15) |
| No | 411 (66.2) |
| Didn’t know | 117 (18.8) |
Table 4: Participants’ general characteristics
Discussion
Dry eye is a major tear deficiency disorder that affects the millions of people worldwide. It is a distressing problem which is often overlooked and under diagnosed. Clinically dry eye can be divided into three stages. In the first stage the patient has symptoms but no signs are present, in the second stage the symptom of first stage along with reversible signs such as small corneal erosions and superficial ulcers, mucous secretion and hyperaemia of nasal and temporal bulbar conjunctiva are present. In third stage patient has symptoms and signs of first and second stage along with irreversible signs such as corneal opacity and ulceration which can be lead to sight threatening corneal complications.[18]
Our results showed that all our sample population suffering from dry eye syndrome. It also shows that most of Saudi adults watch TV or use a mobile phone or computer or any of smart hardware for long periods and daily or almost daily (86.5%), research shows that users often complain of eye strain, eye fatigue, burning, irritation, redness, blurred vision, and dry eyes, among other repetitive strain symptoms.[18]
Results also shows that (59%) of our sample smoke cigarettes or shisha. Smoking, air pollution and have been suggested as risk factors in various studies. Smoking predisposes the eye to tear film instability by its direct irritant action on the eye and represent modifiable risk factors in dry eye causation. Similarly to our results, Xu argued that there is a correlation between smoking and dry eye.[17]
In addition, results show that about half of sample does surgery to correct their eye (56%). Thus, dry eye is recognized to occur following refractive surgery, and our understanding of its etiology and clinical significance is evolving. Decreased corneal sensation has been proposed as the basis of reduction in blinking and lacrimal secretion after laser assisted in situ keratomileusis (LASIK) surgery, both of which may contribute to an aqueous-deficient state. Alternatively, it has been proposed that this symptomatic condition is due to the disruption of trophic sensory support to the denervated region. Also, results showed that people whom drive for long distances shows to be in high prevalence of being having dry eye (49%) and that’s can be explained by the dry air and dust faces them or the exposure for sun and that’s for a long period of time.
With related to dry eye symptoms results showed that some participants suffering from such symptoms; mucus in the form of filaments around the eye or inside it and about 31% reported pain or tingling in their eyes, burning sensation, while about half of adults reported that they desire to itch their eyes (61%). Thus, dryness of the eyes was complained by about 38% of participants. Phadatare reported that the main symptom of dry eyes is dry and gritty feeling in the eyes. [18] The additional symptoms include burning or itching in the eyes, the formation of mucus in and outside the eye.
In addition, results indicated that dusty air (31%) and uses of electronic devices (25.4%) are the most reasons for dry eye symptoms reported by participant, followed by wearing contact lenses (15.9%). Ranjan found that exposure factors like sunlight, excessive wind, smoking, drugs, and air pollution as increase dry eye symptoms.[4] Researches argued the relation between dry eye and the use of electronic devises and the wear of lenses.[5,6]
On the other hand, our results did not show any significant relation between gender or age and dry eye syndrome, this may be because the majority of our sample is female so we couldn’t get a comparison result between men and women regarding the presence of the disease, and because all the sample we studied suffering from the disease. While most studies reported a relation between gender and age and the prevalence of dry eye syndrome, researches argued that women suffering from dry eye more than men and also people with highest ages.[19, 20]
Conclusion
In a conclusion we can said that dry eye syndrome is affected most of people, and that’s related mainly to their daily life activities. In order, recent knowledge about causes, symptoms, and diagnostic tests of KCS provides better opportunities for improving medical management.
Acknowledgement
We would like to express our very great appreciation to Dr. Nizar Alhibshi, Consultant ophthalmology King Abdul Aziz University, Jeddah, for his valuable and constructive supervision during the planning and development of this research work. His willingness to give his time so generously has been very much appreciated.
REFERENCES
- Lemp MA. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. CLAO J 1995;21:221-32.
- Lemp A, Baudouin C, Baum J. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye Work Shop. Ocul Surf 2007;5:75-92.
- Brown M, Brown GC. Utility assessment and dry eye disease. Ophthalmology 2004;111:852-3.
- Ranjan R, Shukla S, Singh VC, Mishra B, Sinha S, Sharma B, et al. Prevalence of Dry Eye and Its Association with Various Risk Factors in Rural Setup of Western Uttar Pradesh in a Tertiary Care Hospital. Open J Prev Med 2016;6:57-63.
- Hikichi T, Yoshida A, Fukui Y, Hamano T, Ri M, Araki K, et al. Prevalence of dry eye in Japanese eye centers. Graefes Arch Clin Exp Ophthalmol 1995;233:555-8.
- Gupta SK, Gupta V, Joshi S, Tandon R. Subclinically dry eyes in urban Delhi: an impact of air pollution? Ophthalmologica 2002;216:368-71.
- Ohashi Y, Ishida R, Kojima T. Abnormal protein profiles in tears with dry eye syndrome. Am J Ophthalmol 2003;136:291-9.
- Kaercher T, Bron A. Classification and diagnosis of dry eye. Dev Ophthalmol 2008;41:36-53.
- Sharma A, Hindman HB. Aging: a predisposition to dry eyes. J Ophthalmol 2014.
- Smith J, Al Beitz J, Begley C, Caffery B, Nichols K, Schaumberg D, et al. The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye Work Shop. Ocul Surf 2007;5:93-107.
- Schaumberg DA, Sullivan DA, Dana MR. Epidemiology of dry eye syndrome. Adv Exp Med Biol 2002;506B:989-98.
- Kassan S, Moutsopoulos HM. Clinical manifestations and early diagnosis of Sjögren syndrome. Arch Intern Med 2004;164:1275-84.
- Gupta N, Prasad I, Jain R, D'Souza P. Estimating the prevalence of dry eye among Indian patients attending a tertiary ophthalmology clinic. Ann Trop Med Parasitol 2010;104:247-55.
- Jamaliah R, Fathilah J. Prevalence of dry eye in University Malaya Medical Centre. Med J Malaysia 2002;57:390-7.
- Onwubiko SN, Eze BI, Udeh NN, Arinze OC, Onwasigwe EN, Umeh RE, et al. Dry eye disease: prevalence, distribution and determinants in a hospital-based population. Cont Lens Anterior Eye 2014;37:157-61.
- Uchino M, Yokoi N, Uchino Y, Dogru M, Kawashima M, Komuro A, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol 2013;156:759-66.
- Xu L, Zhang W, Zhu XY, Suo T, Fan XQ, Fu Y. Smoking and the risk of dry eye: a Meta-analysis. Int J Ophthalmol 2016;18:1480-6.
- Phadatare SP, Momin M, Nighojkar P, Askarkar S, Singh KK. A Comprehensive Review on Dry Eye Disease: Diagnosis, Medical Management, Recent Developments, and Future Challenges. Advances in Pharmaceutics 2015.
- Bakkar MM, Shihadeh WA, Haddad MF, Khader YS. Epidemiology of symptoms of dry eye disease (DED) in Jordan: A cross-sectional non-clinical population-based study. Cont Lens Anterior Eye 2016;39:197-202.
- Ning-Ning L, Lei L, Jun L, Yi-Zhou S. Prevalence of and Risk Factors for Dry Eye Symptom in Mainland China: A Systematic Review and Meta-Analysis. J Ophthalmol 2014.