Drug Utilizing Pattern for Acne Vulgaris in a Tertiary Care Teaching Hospital
Citation: Gupta A. Drug Utilizing Pattern for Acne Vulgaris in a Tertiary Care Teaching Hospital. J Basic Clin Pharma 2017;8:230-234.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@jbclinpharm.org
Abstract
Context: Acne vulgaris is the most common chronic inflammatory skin condition which lasts for many years. Treatment and compliance with regimen is an essential element in overall effectiveness of therapy. In Indian market, various brands of drugs are available for the treatment of acne vulgaris. Aim: To evaluate the drug usage pattern in acne vulgaris and also to estimate the cost difference between various brands of drugs available for treatment of acne vulgaris. Settings and Design: Cross-sectional observational study.
Material and Methods: Data of 183 acne patients attending skin OPD was collected. Physicians and patients were informed and their written consent was taken. Data collected from the prescriptions included demographic profile of patients, drugs prescribed with their dose, route, frequency and duration, average number of drugs. Cost variation amongst the different drugs available for treatment of acne vulgaris was also calculated. Results were expressed in percentage or frequencies. Statistical analysis used: NIL.
Results: Dermatologists had prescribed retinoids both topically and orally in 30% subjects. Azithromycin was the most frequently and initially prescribed systemic antimicrobial. The maximum cost variation was seen with Hydroxyzine (1130.76%) followed by Doxycycline (458.33%).
Conclusions: Prescriptions for acne vulgaris were seen to be according to the guidelines and there was wide per day cost variation in the treatment given to these patients who ranged from Rs. 15.50 to Rs. 155.70/-.
Keywords
Acne vulgaris, prescription trend, cost variation
Introduction
Acne vulgaris is the most common skin condition seen by the dermatologists which occurs most commonly during adolescence, affecting an estimated 80-90% of teenagers. Medications for acne include benzoyl peroxide, antibiotics (either topical or by pill), retinoids, anti-seborrheic medications, anti-androgen medications, hormonal treatments, salicylic acid, alpha hydroxy acid, azelaic acid, nicotinamide, and keratolytic soaps. Early and aggressive treatment is advocated by some to lessen the overall long-term impact to individuals. [1]
Acne is a treatable disease, but the treatment usually lasts for many years and it may influence many aspects of patient’s life. In majority of the cases, the patient’s adherence to treatment is directly dependent on cost of treatment and compliance with treatment regimen is an essential element in overall effectiveness of therapy.
In the Indian market, drugs of various brands are available for the treatment of acne vulgaris. This creates a lot of confusion for the physician to decide the brand of choice for their patients. Literature search revealed very few studies which compared the cost of drugs of different brands for acne vulgaris. [2-4]
This study was planned to evaluate the drug usage pattern in acne vulgaris and also to estimate the cost difference between various brands of drugs available for treatment of acne vulgaris.
Subjects and Methods
The study was started after getting approval from Institutional Ethics Committee. This study was a cross-sectional observational study. Data was collected from Feb 2015 to Jan 2016 by visiting Dermatology OPD for 2 random days per week and viewing the prescriptions during this study period. Sample size calculated considering the number of patients coming to our dermatology OPD for consultation of acne vulgaris per month and the visiting frequency of the investigator was 180 subjects. Our study included total 183 subjects who gave written consent (>18 years of age)/assent (<18 years of age) for viewing their prescriptions/case sheet. Informed written consent was also taken from the dermatologists to view the prescriptions of their patients who came for consultation on acne vulgaris.
Following data was collected:
1. Demographic details of patients: Age, Gender, Education and Occupation.
2. Number of visits for acne consultations and grade of acne vulgaris.
3. Prescribed drug details: Name, Formulations, strength, Dose, Duration, Route of administration, Time of administration and any written instructions given to patients related to drugs.
4. Total Cost of the treatment.
Prescribed drugs were classified according to their pharmacological class. The other details of prescribed drugs like contents, manufacturing company and price were obtained from reference books like CIMS and Drug Today.
Statistical Analysis
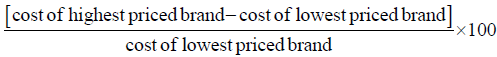
Results were expressed in percentage or frequencies. The appropriateness of acne vulgaris treatment was assessed using American Academy of Dermatology guidelines 2016. The cost difference in the maximum and minimum price of the same drug manufactured by different pharmaceutical companies was calculated. The cost variation amongst the different drugs available for treatment of acne vulgaris was calculated by the formula: [5]
Results
This was an observational cross sectional study in which prescriptions of 183 patients of acne vulgaris attending dermatology OPD of a tertiary care teaching hospital were analysed. Majority of the patients were ≤ 20 years of age (n=80, 43.7%) in whom female patients outnumbered the male patients (F-108, M-75). 46.4% of our study subjects had acne vulgaris for >12 months duration. Of all subjects, 84% patients were diagnosed as Grade II acne vulgaris, 14% as Grade I and only 2% patients were having grade IV disease.
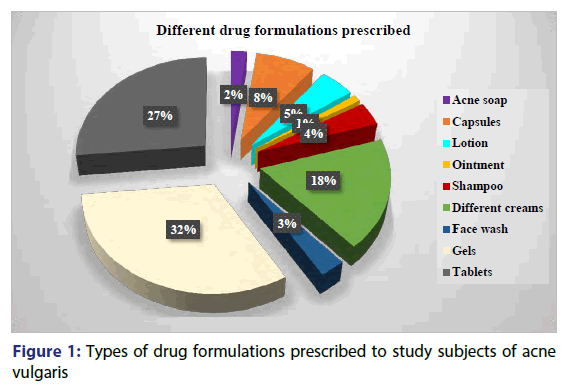
Grade I patients of acne vulgaris were treated with oral antimicrobials and antifungal drugs along with topical antibiotics, retinoid, antibiotics+retinoid combination or Benzoyl peroxide [Table 1]. Treatment with oral retinoids is seen started in the patients from Grade II acne vulgaris along with anti-histaminics, anti-inflammatory drugs and vitamin supplements given orally. Topical steroids alone or in combination with antifungal drug Terbinafine and other miscellaneous agents like natural remedies, face wash; shampoos were also prescribed for patients with grade II acne vulgaris [Table 2]. The treatment of grade IV acne vulgaris differed only by addition of oral steroid (Prednisolone) to the drug list along with same treatment drugs as for grade II acne [Figure 1].
| Drug Category | Oral drugs | Topical agents |
|---|---|---|
| Retinoid 197 (30%) |
Isotretinoin 28 (14%) |
Tretinoin 52 (26%) Adapalene 117 (60%) |
| Antimicrobials 325 (43%) |
Azithromycin 76 (23%) Doxycycline 53 (16%) Minocycline 27 (8%) Cefpodoxime 5 (2%) Amoxicillin 4 (1%) |
Clindamycin 146 (46%) Nadifloxacin 5 (2%) |
| Antifungal 64 (9%) |
Fluconazole 23 (40%) |
Terbinafine 7 (11%) Ketoconazole 21 (33%) |
| Corticosteroids 19 (3%) |
Prednisolone 5 (26%) |
Mometazone 14 (74%) |
| Miscellaneous 194 (26%) |
Antihistaminics (Hydroxyzine, Levocetrizine) Anti-inflammatory (Diclofenac+Serratiopeptidase) Vitamins |
Azelaic acid Allantoin Aloe Vera gel combinations Cetyl+Stearyl Alcohol Benzoyl peroxide Glycolic acid Hydroquinone PABA Zinc Face wash and moisturising / lightening creams |
| FDCs (31%) |
Amoxicillin+Clavulanic acid Diclofenac+Serratiopeptidase |
Adapalene+Clindamycin Aloe Vera+liquid paraffin Mometazone+Terbinafine Allantoin+Clindamycin Nicotinamide+Clindamycin Aloe vera+Calamine Ketoconazole+Zinc shampoo Face wash and moisturising/lightening creams |
Table 1: Categories of drugs used for the treatment of acne vulgaris in the study subjects.
| Category | n (%) |
|---|---|
| Number of prescriptions | 183 |
| Total no. of drugs prescribed | 758 |
| Total no. of drugs prescribed through oral route | 250 (33%) |
| Total no. of drugs prescribed through topical route | 508 (67%) |
| Average no. of drugs prescribed per prescription | 4.14 |
| No. of fixed dose combinations prescribed | 233 (31%) |
Table 2: Analysis of prescriptions for patients of acne vulgaris
Table 3 summarizes the most frequently prescribed drugs for the treatment of acne vulgaris in the study subjects with minimum and maximum cost of their formulations available in the Indian market. Percentage cost variation has been calculated for these drugs and tablet Hydroxyzine shows maximum cost variation (1130.76%) followed by Doxycycline (458.33%). The least cost variation was seen with the Mometazone+Terbinafine (4.76%) cream formulation. In our study, mean cost of treatment was for acne vulgaris Rs. 56.30/- per day with minimum cost of Rs. 15.50/- and maximum Rs. 155.70/- per day.
| Drugs | Formulation | Min | Max | Percentage Cost Variation |
|---|---|---|---|---|
| Adapalene | Gel | 75 | 200 | 166.66 |
| Adapalene+Clindamycin | Gel | 79 | 214 | 170.88 |
| Azelaic Acid (15 gm) | Cream | 110 | 135 | 22.72 |
| Benzol Peroxide | Gel | 63 | 95 | 50.79 |
| Clindamycin | Gel | 57 | 149 | 161.40 |
| Clindamycin+Nicotinamide | Gel | 39 | 93 | 138.46 |
| Doxycycline | Tab | 0.6 | 3.35 | 458.33 |
| Hydroxyzine | Tab | 6.5 | 80 | 1130.76 |
| Hydroxyquinone | Cream | 50 | 66 | 32 |
| Isotretinoin | Cap | 87 | 290 | 233.33 |
| Ketoconazole | Cream | 70 | 139 | 155.71 |
| Ketoconazole+Pyrithione+Aloe Vera | Shampoo | 70 | 145 | 107.14 |
| Minocycline | Tab | 128 | 230 | 79.68 |
| Mupirocin | Ointment | 70 | 101 | 44.28 |
| Mometazone | Cream | 68 | 99 | 45.58 |
| Mometazone+Terbinafine | Cream | 105 | 110 | 4.76 |
| Nadifloxacin | Lotion | 40.6 | 66 | 62.56 |
| Prednisolone | Tab | 13.7 | 30 | 118.97 |
| Tretinoin | Cream | 39 | 108 | 176.92 |
| Tretinoin | Gel | 49.9 | 113 | 126.45 |
Table 3: Percentage cost variation among various anti-acne drugs prescribed in the study
Discussion
Acne is known to be a disease of the adolescents affecting approximately 85%-90% of the teenagers. [6,7] It is most commonly present between the ages of 10 and 13 years in both sexes with the mean age of onset of acne being 11 years in girls and 12 years in boys. [8,9] Acne is now presenting earlier and lasting longer. [10] The results of this study shows that majority of the patients were of ≤ 20 years of age (n=80, 43.7%).
The average age of the patients during the study period was 22.5 years.
When we considered the total number of study participants, female patients outnumbered the male patients (F-108, M-75). But this trend was exactly the opposite in adolescents <20 years age group where there were more males (58%) than females (42%). As we advanced to the higher age groups, number of female patients increased in them. In the age group of 21-25 years, there were 62% female’s verses 38% of males and so on. The >30 years age group consisted of all female patients (100%). Post‐adolescent acne, both persistent and late onset, is more common in women than in men. [10-12]
In our study majority of the patients (84%) were suffering from Grade II acne vulgaris. This result is in consistence with the observation made in a study conducted by Patro et al. in Odisha where around 60% of cases were of grade II. Another study done by Swati et al. also found a preponderance of grade II [13] (80%) acne presenting to the department of dermatology. Studies have shown that, adult acne in Indian patients usually presents as inflammatory papules and pustules of mild to moderate severity (Grade II). [12]
The various categories of drugs prescribed to these patients of acne vulgaris included retinoids, antimicrobials, antifungals, benzoyl peroxide, corticosteroids and certain miscellaneous agents like anti-histaminics, anti-inflammatory drugs, shampoos, face wash, moisturising / lightening creams, etc.
We found that retinoids (Tretinoin, Adapalene, and Isotretinoin) were prescribed both topically as well as orally in total 30% of the patients. Topical tretinoin and adapalene are recommended as monotherapy in primarily comedonal acne, or in combination with topical or oral antimicrobials in patients with mixed or primarily inflammatory acne lesions. These can also be safely used in the management of preadolescent acne in children. Oral isotretinoin was recommended in our study patients for the treatment of some cases of Grade II and all cases of Grade IV acne. Isotretinoin is appropriate for the treatment of moderate acne that is treatment-resistant or for the management of acne that is producing physical scarring or psychosocial distress. [12] Low-dose isotretinoin can be used to effectively treat acne and reduce the frequency and severity of medication-related side effects. [14]
Topical antimicrobials (e.g., erythromycin and clindamycin) are effective acne treatments, but are not recommended to be prescribed alone because of the risk of development of bacterial resistance. They should always be given along with another topical or systemic antimicrobial; retinoids (oral or topical); benzoyl peroxide, etc. [14] Similar prescription trend was seen in the study which speaks about the rationality of prescriptions for acne vulgaris in this set up.
Regarding systemic antimicrobials use, American Academy of Dermatologists have proposed that systemic antimicrobials should be recommended in the management of moderate to severe acne and forms of inflammatory acne that are resistant to topical treatments. They also proposed doxycycline and minocycline are more effective than tetracycline, but neither is superior to each other whereas oral erythromycin and azithromycin can be effective in treating acne but its use should be limited to those who cannot use tetracycline. [14] In our study, we found that Azithromycin was the most frequently prescribed oral antimicrobial which was preferred to be prescribed before trying out tetracycline antimicrobials. This observation is in contrast to the recommendations by the American Academy of Dermatologists (2016). We sought the explanation for this deviation in practice of using antimicrobials from the consulting dermatologists. As tetracyclines are associated with photosensitivity reactions and gastrointestinal upset more often than that with Azithromycin, they preferred to use Azithromycin over tetracycline group of drugs in acne treatment. Additionally, in mild and non-inflammatory acne they prescribed Azithromycin over tetracycline as it is known to be safe and effective with better patient compliance. [15-17]
In our study, we found that antifungals were prescribed orally or topically in some cases. This may be because of infection by pityrosporum species leading to the development of folliculitis, an infection of the hair follicles. This fungus can be found in small numbers in stratum corneum and hair follicle in up to 90% individuals without any disease. [18,19] As acne vulgaris and pityrosporum folliculitis coexist it may be necessary to combine antifungal treatments along with typical acne medications. Traditional acne therapies, especially antimicrobials given alone can alter normal flora and worsen this condition. [20] We came across 39 such prescriptions where antifungals were given along with antimicrobials.
Benzoyl peroxide or combinations with erythromycin or clindamycin are effective in acne treatment and prevention of bacterial resistance. These are recommended as monotherapy for mild acne, or in conjunction with a topical retinoid, or systemic antibiotic therapy for moderate to severe acne. [14] Similar use was noted in our study where Benzoyl peroxide was prescribed in all grades of acne either alone or in combination with the above said antimicrobials.
As far as prescription of corticosteroids for acne vulgaris is concerned, in our study, it was recommended for some patients of Grade II topically (Mometasone+Terbinafine) and for all patients of Grade IV acne orally (prednisolone) as well as topically. It was found that the topical steroid+antifungal preparation were prescribed to patients who were suffering from both acne and tinea infections. Oral corticosteroids were preferably given to patients who had severe inflammatory acne which is also recommended by the American Academy of Dermatologists (2016). [14,20,21]
Indian markets are flooded with a huge number of branded formulations which are available for every drug molecule. But there is always a pricing difference between the different brands of the same formulation. Pharmacists may not dispense the same brand as prescribed by the doctor and try to substitute it with other alternatives, quoting the reason of non-availability. This is often done with vested interest for economic gains as some brands have a higher profit margin.
Due consideration must be placed on pricing of drugs in the Essential Drug List to increase their accessibility to common people. Drug Price Control Order (DPCO) appears to be an effective tool to keep in rein the drug prices. [22]
In our study, we had compared the cost of different brands of antiacne drugs. The drug prices available in CIMS and Drug Today were compared, as they are commonly referred source of drug information and are updated regularly. It is observed from our results that there is a wide (from 4.76% to 1130.76%) variation in prices of these drugs manufactured by different pharmaceutical companies. The maximum cost variation is seen with Hydroxyzine (1130.76%) followed by Doxycycline (458.33%), This might be due to the fact that the drug is manufactured by many pharmaceutical companies and hence available options may vary much in their prices and the least cost variation is seen with the Mometazone+Terbinafine (4.76%) combination cream [Table 3]. This might be due to the fact that the drug is not yet manufactured by many pharmaceutical companies and hence available options do not vary much in their prices. A study on percentage cost variation of anti-diabetic drugs done by Jadhav et al. concludes that as the number of manufacturing companies increases, the percent price variation also increases. [23,24]
The reasons for this price variation have been worked-on by many researchers and could be as follows: [25-30]
1. The existing market structure of the pharmaceutical industry
2. Asymmetry of information or imperfect information
3. Industry costs
4. Government regulations and pricing policies
5. Costs of raw supplies, distribution and promotion
6. Economic goals of the parent company, target return on investment.
It is felt that physicians could provide better services and reduce costs of drugs if information about drug prices was readily available. In our study, mean cost of treatment was Rs.56.30/- per day with minimum cost of Rs.15.50/- and maximum was Rs.155.70/-. Cost is a crucial issue in patient’s adherence especially for patients with chronic disease as the treatment period could be prolonged. [31] Increasing medication adherence may produce a greater benefit to the patient’s disease than improvements in specific medical therapy.
Conclusion
The study revealed that the prescriptions for acne vulgaris were found to be according to the standard guidelines but there was a wide per day cost variation in the treatment given to these patients who ranged from Rs. 15.50 to Rs. 155.70/-.
REFERENCES
- Goodman G. Acne and acne scarring: the case for active and early intervention. Aust Fam Physician 2006 Jul;35:503-4.
- Bossuyt L, Bosschaert J, Richert B, Cromphaut P, Mitchell T, Al Abadie M, et al. Lymecycline in the treatment of acne: an efficacious, safe and cost-effective alternative to minocycline. Eur J Dermatol: EJD 2002;13:130-5.
- Narwane SP, Patel TC, Shetty YC, Chikhalkar SB. Drug utilization and cost analysis for common skin diseases in dermatology OPD of an Indian tertiary care hospital-A prescription survey. Br J Pharm Res 2011;1:9.
- Balkrishnan R, Kulkarni AS, Cayce K, Feldman SR. Predictors of healthcare outcomes and costs related to medication use in patients with acne in the United States. Cutis. 2006;77:251-5.
- Shankar PR, Subish P, Bhandari RB, Mishra P, Saha AC. Ambiguous pricing of topical dermatological products: a survey of brands from two South Asian countries. J Pak Assoc Dermatol 2006;16:134-40.
- Stathakis V, Kilkenny M, Marks R. Descriptive epidemiology of acne vulgaris in the community. Australas J Dermatol 1997;38:115-23.
- Kraning KK, Odland GF. Prevalence, morbidity, and cost of dermatological diseases. J Invest Dermatol 1979;73:395-513.
- Dreno B, Poli F. Epidemiology of acne. Dermatology 2003;206:7-10.
- Schäfer T, Nienhaus A, Vieluf D, Berger J, Ring J. Epidemiology of acne in the general population: the risk of smoking. Br J Dermatol 2001;145:100-4.
- Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D. Rook's Textbook of Dermatology. John Wiley & Sons. 9th edn. 2016;90.1-90.65.
- Khunger N, Kumar C. A clinico-epidemiological study of adult acne: is it different from adolescent acne. Indian Indian J Dermatol Venereol Leprol 2012;78:335.
- Swati G, Kusagur MS. A Clinico-Epidemiological Study of Acne in Adults. IJSR 2015;4:822-5.
- Patro N, Jena M, Panda M, Dash M. A Study on the Prescribing Pattern of Drugs for Acne in a Tertiary Care Teaching Hospital in Odisha. JCDR 2015;9:WC04.
- Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol 2016;74:945-73.
- Fernandez-Obregon AC. Azithromycin for the treatment of acne. Int J Dermatol 2000;39:45-50.
- Bardazzi F, Savoia F, Parente G, Tabanelli M, Balestri R, Spadola G, et al. Azithromycin: a new therapeutical strategy for acne in adolescents. Dermatol Online J 2007;13:4.
- Kapadia N, Talib A. Acne treated successfully with azithromycin. Int J Dermatol 2004;43:766-7.
- Faergemann J, Johansson S, Bäck O, Scheynius A. An immunologic and cultural study of Pityrosporum folliculitis. J Am Acad Dermatol 1986;14:429-33.
- Hill MK, Goodfield MJ, Rodgers FG, Crowley JL, Saihan EM. Skin surface electron microscopy in Pityrosporum folliculitis: the role of follicular occlusion in disease and the response to oral ketoconazole. Arch Dermatol 1990;126:1071-4.
- Ayers K, Sweeney SM, Wiss K. Pityrosporum folliculitis: diagnosis and management in 6 female adolescents with acne vulgaris. Arch Pediatr Adolesc Med 2005;159:64-7.
- Darley CR, Moore JW, Besser GM, Munro DD, Kirby JD. Low dose prednisolone or oestrogen in the treatment of women with late onset or persistent acne vulgaris. Br J Dermatol 1983;108:345-53.
- Das SC, Mandal M, Mandal SC. A Critical Study on Availability and Price Variation Between Different Brands: Impact on Access to Medicines. Indian J Pharm Sci 2007;69:160-3.
- Jadhav NB, Bhosale MS, Adhav CV. Cost analysis study of oral antidiabetic drugs available in Indian market. International Journal of Medical Research & Health Sciences 2013;2:63-9.
- Karve AV, Chattar KB. Cost analysis study of oral antihypertensive agents available in Indian market. Int J Basic ClinPharmacol 2014;3:479-83.
- Sarkar PK. A rational drug policy. Indian J Med Ethics 2004;12;30-5.
- Roy V, Rewari S. Ambiguous drug pricing: a physician’s dilemma. Indian J Pharmacol 1998; 30:404-7.
- Wertheimer AI, Grumer SK. Overview of international pharmacy pricing. Pharmacoeconomics 1992;2:449-55.
- Berki SE, Richard JW, Weeks HA. The mysteries of prescription pricing in retail pharmacies. Medical care 1977;15:241-50.
- Rataboli PV, Dang A. Antimicrobial price variation: Conundrum of medical profession!. J Postgrad Med 2007;53:72-4.
- Dawadi S, Rao BS, Khan GM. Pattern of antimicrobial prescription and its cost analysis in respiratory tract infection. J Sci Eng Technol 2005;1:1-9.
- Ponnusankar S, Surulivelrajan M, Anandamoorthy N, Suresh B. Assessment of impact of medication counselling on patients’ medication knowledge and compliance in an outpatient clinic in South India. Patient Educ Couns 2004;54:55-60.