Drug utilization patterns in the emergency department: A retrospective study
- *Corresponding Author:
- Dr. K. A. Al Balushi
Department of Pharmacology and Clinical Pharmacy, College of Medicine and Health Sciences, Sultan Qaboos University, P. O. Box 35, Postal Code 123, Al-Khod, Sultanate of Oman.
E-mail: mme51@squ.edu.om
Abstract
Objectives: The aim of this study was to assess the prescribing trends and costs of drugs in the emergency department (ED) at Sultan Qaboos University Hospital (SQUH), a tertiary care hospital, in Muscat, the Sultanate of Oman. Materials and Methods: This was a retrospective cross‑sectional study of all patients (n = 300) who attended the ED at SQUH in May 2012. Analyses were performed using descriptive and univariate statistics. Results: The average age of patients was 34 ± 19 years. The average number of drugs prescribed per patients was 3.2 ± 1.9 and the majority of the patients (n = 78; 26%) received two drugs. The most common route of drug administration was the oral route (n = 481; 51%) followed by parenterally (n = 357; 38%). Non‑steroidal anti‑inflammatory drugs (NSAIDs) were the most commonly prescribed class of drugs (38%) followed by the gastro‑intestinal tract drugs (19%) and central nervous system drugs (13%). The average cost per prescription was 242 ± 632 US$. Morphine had the highest cost (1885 US$) followed by cefuroxime (1404 US$) and filgrastim (939 US$) over the 1‑month period. There was a significant positive correlation between hospital cost and age (P < 0.001), duration of stay at the ED (P = 0.008) and emergency types (P < 0.001). Conclusion: NSAIDs were the most frequent class of drugs administered to patients. Highest number of drugs was prescribed for cardiovascular diseases followed by respiratory and gastrointestinal diseases. Anti‑infective drugs cost was the highest among all other classes. The results of the present study are attempts to highlight the importance of strategies that have to be implemented to optimize medication use at the ED.
Keywords
Drug, emergency, pattern, utilization
Introduction
Problems associated with drug prescriptions are not uncommon world-wide. These include mainly medications errors and adverse drug events. [1] A meta-analysis of 35 studies between 1990 and 2005 indicated that medication errors occurred in a mean of 5.7% of all drug administration episodes while adverse drug events affected 6.1 patients per 100 hospitalized. [1] Many factors are involved in drug prescription errors including polypharmacy, lack of sufficient pharmacological knowledge, errors in patients’ charts or documentation by nurses, inadequate pharmacy service, being a female, age >65 years, renal excretion of drugs, drugs with narrow therapeutic index and the use of anticoagulants or diuretics. [1] Furthermore, several studies in the United States have consistently reported adverse drug events ranging from 3% to 12%. [2] These studies indicate that 1.5-3% of all adverse drug events occur in the emergency department (ED). However, the EDs had the highest proportion of prevalence of preventable (70-82%) errors. [2]
Patients come to the ED for evaluation of emergent or urgent conditions for after-hours medical care, or by referral from their primary physician. In the ED, doctors face urgent and sever cases that need to be treated quickly with high quality. This creates a challenge for physicians to initiate and select appropriate drugs for the patient. Furthermore, the unique operating characteristics of ED make the ED vulnerable to medical errors including medication errors and adverse drug events. Many factors, either intrinsic or extrinsic, influence the quality of health care in the ED. These include: High levels of activity, high cognitive load, high decision density, high levels of diagnostic uncertainty, inexperience of physicians and nurses, distractions, narrow time window and shift work. [2]
The World Health Organization (WHO) compiled a set of core drug use indicators that are useful for studying patterns of drug prescribing in health care facilities. [1] The WHO also stated that: “Rational use of drugs requires that patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements for an adequate period of time and at the lowest cost to them and their community.” [3] The WHO core indicators for drug utilization include: Average number of drugs per encounter, percentage of drugs prescribed by generic name, percentage of encounters with an antibiotic, percentage of encounters with an injection, percentage of drugs prescribed from the essential drug list. [4] Another tool used to control and contrast the rational use of drugs is the hospital’s pharmaco-therapeutic guide, which is used and studied by the pharmaceutical and therapeutics commission of any hospital.
In contrast, irrational use of drugs refers to the distribution or consumption of drugs in ways that negate or reduce their efficacy or in situations where they are unlikely to have the desire effect. [5] Irrational prescription of drugs leads to unproductive and risky treatment and poses a major risk of present day medical practice. The problem of irrational drug prescription is not restricted to developing countries as there is evidence from many developed countries on the inappropriate use of drugs. [6] Appropriate medication use is of both clinical and economic significance to any health system and should be given adequate attention. [7]
Drug utilization research is a component of medical audit that plays an important role in pharmaco-epidemiological studies. This is because it reports the extent, quality, determinants and outcome of drug exposure. In addition, it helps in assessing rational usage and cost control of various medications used in the hospital. Pharmaco-epidemiological studies detailing prescribing patterns of physicians are very few from developing countries. [8] Currently, there is limited local data on the prescribing habits of doctors at the ED. The aim of this study was to assess drug prescribing trends, average number of drugs per prescription, the WHO core indicators for drug utilization and prescription cost during patients’ visits at the ED at Sultan Qaboos University Hospital (SQUH).
Materials and Methods
Study setting
This study was conducted at the ED of SQUH, a tertiary care hospital, in Muscat, the Sultanate of Oman. The SQUH has a total of 557 beds while the ED has 28 beds. The ED is visited by approximately 60,000 patients annually.
Study design and subjects
This was a retrospective cross-sectional study of all patients (n = 300) who attended the ED at SQUH in May of 2012. The subjects included both Omanis and non-Omanis from all age groups. The hospital information system was used to extract relevant patients’ information.
WHO core drug prescribing indicators
The WHO prescribing indicators mentioned above were measured retrospectively from the hospital’s medical records. No information was collected about the signs and symptoms of diseases as this is not a requirement as per the WHO guidelines in this type of study. [4]
Statistical analysis
Descriptive statistics were used to describe the data. For categorical variables, frequencies and percentages were reported. For continuous variables, means and standard deviations (±SD) were reported. The cost of medications was tested for normal distribution using one-sample Kolmogorov-Smirnov test. The association between drugs cost and patient’s gender was conducted by Mann-Whitney Test and between the drug cost and type of emergency and patient’s outcome. However, the correlation between drug cost and duration of stay at the ED and patient’s age was performed using Spearman’s correlation coefficient. An a priori two-tailed level of significance was set at the 0.05 level. Statistical analyses were conducted using STATA version 12.1 (STATA Corporation, College Station, TX, USA).
Ethical approval
Ethical approval for the study was obtained through the Medical research and Ethics Committee at the College of Medicine and Health Sciences.
Results
General characteristics of the patients
Among the recruited patients, 155 (52%) were males and 145 (48%) were females. The average age of the patients was 34 ± 19 years. Only 15% (n = 45) of patients were referred to other departments for further management. The characteristic of the patients are shown in Table 1.
| Total number of patients (N) | 300 |
| Age, mean±SD, (years) | 34±19 |
| Sex (n, %) | |
| Female | 145 (48) |
| Male | 155 (52) |
| Weight, mean±SD, (kg) | 51±28 |
| Duration of stay at ED, hours (median, IQR) | 3.38 (1.5-4.5) |
| Number of drugs prescribed per patient (mean±SD) | 3.16±1.89 |
| Patient’s outcome % | |
| Discharged | 85 |
| Referred to other departments | 15 |
ED: Emergency department, IQR: Interquartile range, SD: Standard deviation
Table 1: Summary of the characteristics of the 300 patients in the ED at Sultan Qaboos University Hospital
Drug utilization pattern among patients
The total number of prescriptions for the 300 patients over the month was 939. The average number of drugs prescribed per patients was 3.16 ± 1.89. The distribution of drugs among patients included in this study was: 55 (18%) patients received one drug; 78 (26%) patients received two drugs; 60 (20%) patients received three drugs; 47 (16%) patients received four drugs; 30 (18%) patients received five drugs; and the rest received more than five drugs (10%). There were no patients who did not receive no drug. The majority of drugs were administered by the oral route (n = 481; 51%) followed by the parenteral route (n = 357; 38%) and then topical route (n = 54; 6%).
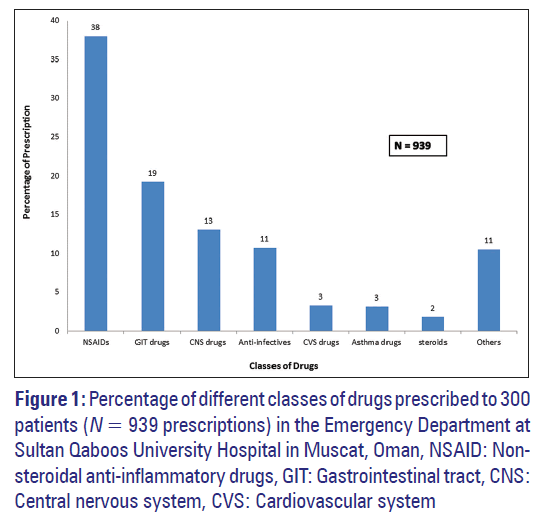
A total of 103 drugs, belonging to seven categories, were prescribed. Figure 1 shows the most frequently administered classes of drugs. The non-steroidal anti-inflammatory drugs (NSAIDs) were the most commonly prescribed class of drugs (38%) followed by the gastro-intestinal tract (GIT) drugs (19%) and central-nervous system (CNS) drugs (13%). Table 2 outlines the top 10 drugs prescribed to all patients. Paracetamol was the most commonly prescribed drug (n = 195; 21%) followed by morphine (n = 67; 7%) and diclofenac (n = 62; 7%).
| Name of drug | N | Percentage |
|---|---|---|
| Paracetamol | 195 | 21 |
| Morphine | 70 | 7 |
| Diclofenac | 62 | 7 |
| Co-codamol (paracetamol and codeine) | 29 | 3 |
| Ranitidine | 49 | 5 |
| Augmentin (amoxicillin and clavulanate potassium) | 45 | 5 |
| Ibuprofen | 39 | 4 |
| Metoclopramide | 36 | 4 |
| Ipratropium | 19 | 2 |
| Salbutamol | 18 | 2 |
| Others | 377 | 40 |
| Total | 939 | 100 |
ED: Emergency department
Table 2: The top 10 drugs prescribed to 300 patients in the ED at Sultan Qaboos University Hospital in Muscat, Oman
Table 3 shows the distribution of drug classes across various emergency types, indicating that NSAIDs and CNS drugs were mostly prescribed for hematological patients (56 and 54 cases, respectively), whereas asthma drugs and steroids were mostly prescribed for respiratory patients (21 and 6 cases, respectively).
| Drugs (n) | Anti-infective | Asthma drugs | CNS drugs | CVS drugs | GIT drugs | NSAID | Steroid | Others |
|---|---|---|---|---|---|---|---|---|
| Hematological | - | - | 54 | - | 1 | 56 | - | 10 |
| Musculoskeletal | 2 | 1 | 15 | 1 | 5 | 46 | - | 15 |
| Infection | 62 | 2 | 5 | - | 12 | 50 | 2 | 13 |
| Trauma | 4 | - | 12 | 1 | 1 | 32 | - | 12 |
| CVS | 1 | - | 2 | 21 | 6 | 11 | - | 1 |
| CNS | - | - | 12 | 1 | 2 | 16 | 1 | 1 |
| Metabolic | - | - | - | 1 | 4 | 5 | 1 | 3 |
| Respiratory | 7 | 21 | - | 1 | 2 | 16 | 6 | 10 |
| Renal | 9 | - | 6 | - | 8 | 26 | - | 7 |
| Gastrointestinal | 12 | 4 | 13 | 1 | 125 | 55 | 1 | 16 |
| Others | 4 | 2 | 4 | 4 | 15 | 44 | 6 | 11 |
| Total | 101 | 30 | 123 | 31 | 181 | 357 | 17 | 99 |
CVS: Cardiovascular system, CNS: Central nervous system, NSAID: Non-steroidal anti-inflammatory drug, ED: Emergency department, GIT: Gastro-intestinal tract
Table 3: Distribution of drug classes across various emergency types among 300 patients in the ED at Sultan Qaboos University Hospital in Muscat, Oman
Figure 1: Percentage of different classes of drugs prescribed to 300
patients (N = 939 prescriptions) in the Emergency Department at
Sultan Qaboos University Hospital in Muscat, Oman, NSAID: Nonsteroidal
anti-inflammatory drugs, GIT: Gastrointestinal tract, CNS:
Central nervous system, CVS: Cardiovascular system
WHO core indicators of drug utilization pattern
The WHO core prescribing indicators are shown in Table 4.
| Indicator | value |
|---|---|
| Average number of drugs per encounter | 3.16±1.89 |
| Percentage of encounters with an antibiotic | 10% |
| Percentage of encounters with an injection | 38% |
| Percentage of drugs prescribed from the essential drug list | 58% |
ED: Emergency department, WHO: World Health Organization
Table 4: WHO core drug prescribing indicators in the study population (n=300) at the ED at Sultan Qaboos University Hospital in Muscat, Oman
Drug prescribing cost at the ED at SQUH
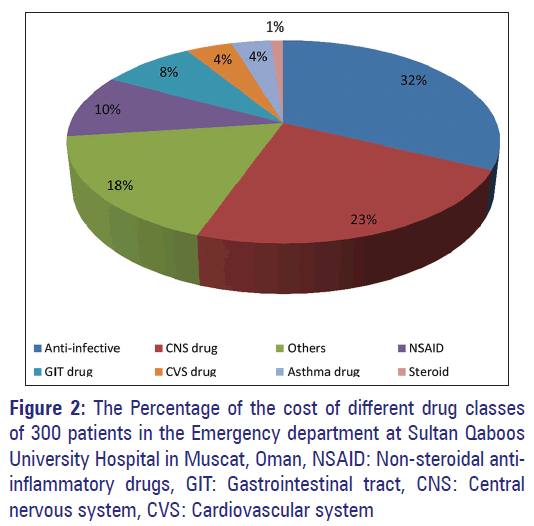
As shown in Table 5, the average cost per prescription was 242 ± 631 US$. Table 6 shows the top 10 drugs that account for the highest cost among all drugs prescribed. Morphine had the highest cost (1884 US$) followed by cefuroxime (1404 US$) and filgrastim (940 US$). Figure 2 represents the percentage of the cost of different drug classes showing that anti-infective drugs incurred the highest cost (2810 US$) followed by CNS drugs (2004 US$).
| Indication | n | Percentage | Average no. of drugs (mean±SD) | Average cost/patient (US$) |
|---|---|---|---|---|
| Hematological | 54 | 18.00 | 3.13±2.02 | 3.80±2.17 |
| Gastrointestinal | 51 | 17.00 | 3.39±2.32 | 72.98±328.61 |
| Infection | 45 | 15.00 | 3.27±1.56 | 23.69±23.89 |
| Musculoskeletal | 30 | 10.00 | 3.27±1.66 | 20.46±61.72 |
| Trauma | 28 | 9.33 | 2.61±1.20 | 9.67±27.25 |
| Respiratory | 17 | 5.67 | 3.41±2.45 | 23.37±27.87 |
| Renal | 16 | 5.33 | 3.25±1.84 | 14.98±18.33 |
| CNS | 13 | 4.33 | 2.85±1.77 | 32.08±77.09 |
| CVS | 10 | 3.33 | 3.70±1.49 | 8.48±5.25 |
| Metabolic | 6 | 2.00 | 2.17±1.60 | 18.49±34.29 |
| Others | 30 | 10.00 | 3.00±2.08 | 13.55±22.00 |
| Total | 300 | 100 | 3.16±1.89 | 241.54±631.49 |
CVS: Cardiovascular system, CNS: Central nervous system, SD: Standard deviation, ED: Emergency department, US: United States
Table 5: Drug indications, prescribing trends and prescription cost in the ED at Sultan Qaboos University Hospital in Muscat, Oman
| Drug name | Cost (US$) |
|---|---|
| Morphine | 1886 |
| Cefuroxime | 1404 |
| Filgrastim | 940 |
| Tazocin (piperacillin and tazobactam) | 580 |
| Paracetamol | 396 |
| Celecoxib capsule | 356 |
| Augmentin (amoxicillin and clavulanate potassium) | 345 |
| Lactulose solution | 284 |
| Salbutamol | 274 |
| Ciprofloxacin | 213 |
ED: Emergency department
Table 6: The top 10 drugs’ cost of prescribing for 300 patients in the ED at Sultan Qaboos University Hospital in Muscat, Oman
Correlation of drug utilization pattern and cost with different patients’
Parameters
There was no significant association between the hospital cost and patient’s gender (P = 0.730) and clinical outcome (P = 0.958). However, there was a significant correlation between the hospital cost and age (older patients had higher medication cost; P < 0.001), duration of stay at the ED (as the hospital stay increases so too was the cost; P = 0.008) and emergency types (higher cost was associated with infection; P < 0.001).
Discussion
Studying drug utilization pattern in the ED provides a means of assessing drug prescribing trends, efficiency and cost-effectiveness of hospital formularies. To the best of our knowledge, this is the first study in Sultanate of Oman to analyze drug utilization patterns in the ED. The mean age of the patients was 34 ± 19 years and 155 (52%) were males. The average number of drugs per prescription, which is an important index of the standard of prescribing, was 3.16 ± 1.89, with a significant number of the patients in this study (26%) receiving at least two drugs per episode. Cardiovascular diseases had the highest average number of drugs per prescription (3.70 ± 1.49). The average number of drugs per prescription is higher than the WHO recommended average number of drugs per prescription of 2.0. [9]
Two studies conducted in India (n = 200 and n = 259) showed an average number of drugs per prescription of 4.2 and 3.3, respectively. [8-10] In these two studies, cardiovascular disease and alcoholic liver disease had the highest average number of drugs per prescription (5.4 and 3.9, respectively). Another study conducted in Spain (n = 669) showed an average number of drugs per prescription of 1.7. [11] In addition, a study on elderly patients (n = 124) presented to the ED in the USA found an average number per prescriptions of 8.6 (range 0-21). [12] One reason for the higher average number of drugs per prescription in USA compared with the WHO standards is that physicians tend to administer polypharmacy during the initial contact with patient while the diagnosis is not yet confirmed and waiting for laboratory results. Despite this, keeping the mean number of drugs per prescription to as low as possible is always preferable to reduce the risk of drug-drug interactions, development of drugs resistance and adverse drug events.
This study demonstrated a high use of NSAIDs in the ED and this could be explained by the large therapeutic range as shown in Table 3 of this class, especially their usage as analgesics. Furthermore, the reason for high indication of morphine use could be explained by the fact that most patients that visited the ED during the study period were hematological cases (18%; n = 54) having mainly sickle cell disease crisis which required morphine to manage their crisis [Table 3]. This study also showed GIT drugs as the second most commonly prescribed medications (19%) with ranitidine being the most commonly prescribed drug of this class (5%) [Table 2]. This could be reflected by the fact that GIT cases represent 17% (n = 51) of all drug indications in the study [Table 5].
A study evaluated the use of drugs across the different indications in the ED in India (n = 200 patients; 629 prescriptions) and found that antibiotics were the most commonly prescribed drugs (22%) followed by NSAIDs (12%) and a class of GIT drugs called proton pump inhibitors (12%). [12] In contrast to our study, the most common indication for drug prescription in the Indian study was infection (19%), while infection was the third most common indication for drug prescription in our study (15%). Paracetamol was also the most commonly prescribed drug (10%) in a study conducted at the ED in Spain, [11] which is similar to our study results, followed by ibuprofen-an NSAID-(9%) and omeprazole (7%). However, in the Spanish study, [11] the most common indication for drug prescribing was the GIT and metabolism (22%) followed by blood and hematopoietic system (2%), which is almost similar to our data.
In our study, the highest average number of drugs per prescription was for cardiovascular disease (3.70 ± 1.49) followed by respiratory disease (3.41 ± 2.45) and gastrointestinal disease (3.39 ± 2.32). In the Indian study, [10] the average number of drugs per prescription was highest in the cardiovascular disease (5.4 ± 1.2) followed by the central nervous system (4.5 ± 1.0) and renal disease (4.2 ± 0.9).
Cost analysis is an important part of drug utilization research. In our study, anti-infective drugs’ cost (2810 US$) was the highest among all drug classes prescribed followed by CNS drugs (2004 US$) and NSAIDs (878 US$) [Figure 2]. This high cost of these classes was due to the high frequency of drugs prescription of these classes as shown in Table 3. Moreover, most patients came to the ED with hematological, gastrointestinal and infectious diseases which require prescription of these classes of drugs. The total cost of all drug classes was 8690 US$ over the 1-month period and the average cost per prescription was 242 ± 631 US$. In a study conducted in India, [10] the mean cost per prescriptions was 784 ± 134 INR (14 ± 2.4 US$). It should be kept in mind that in order to have a realist view on the total cost of ED visits, other aspects of health care such as investigations, stay in hospital and other intangible costs should be calculated. These aspects were not part of the objectives of this study.
The WHO core indicators of prescribing practices measure the performance of health care providers in several key dimensions related to the appropriate use of drugs. In our study, the average number of drugs per prescription was 3.16 ± 1.89, the percentage of antibiotics use was 10%, the percentage of injectable drug use was 38% and about 58% of drugs were prescribed from the WHO essential drug list [Table 4]. Several drug use studies using these standard drug-use indicators have been performed in many developing countries under the supervision of the WHO to provide ideal values for each indicator (more details can be found in Hogerzeil et al. 1993 and in the WHO manual [4,13]). The average number of drugs per prescription ranged from 1.3 to 3.8. In these studies, the percentage of antibiotics use ranged from 25% to 63% while the percentage of injectable drug use ranged from 0.2% to 48% respectively. Furthermore, some of these studies showed that about 85-88% of drugs prescribed were from the WHO essential drug list. [4]
Our study showed that there was a significant association between the hospital cost and age. Older patients had higher medication cost because as a person gets older he/she are more prone to have variants of diseases as well as chronic diseases with their complications that require further medication management. Moreover, duration of stay in the ED had a significant association with the hospital cost. As the hospital stay increases so too was the cost because long stays mean further investigations and management that are required for the patient. Furthermore, there was also a significant association between the hospital cost and emergency types.
This study is not without limitations. No power analysis was performed in this study and one could not be certain that our sample size (n = 300) was a representative sample of the general Omani population. However, the sample size was in accordance with WHO recommendation for practice assessment in individual facilities which requires that a minimum of 100 samples per facility should be collected for the purpose of evaluation. [9,13] This sample size will give a 95% confidence interval of within 10% for the individual result. [13] Furthermore, since this study was performed in only 1 month, it could not have captured seasonal variations, which could have affected prescribing patterns.
Conclusion
The average number of drugs prescribed per patients in the ED over the 1 month period was 3.16 ± 1.89. NSAIDs were the most frequently class of drugs administered to the patients followed by GIT drugs. The highest number of drugs was prescribed for cardiovascular system diseases followed by respiratory and gastrointestinal. Anti-infective drug cost was the highest among all other classes followed by CNS drugs.
The results of this type of studies highlight the importance of strategies that have to be implemented to optimize medication use at the ED. These include ensuring that all persons involved in the medication process have good pharmacological knowledge, computerization of the entire medication process and engagement of clinical pharmacists in such process. The importance of these strategies should be emphasized in medical curricula and continuing medical education of health professionals.
References
- Krähenbühl-Melcher A, Schlienger R, Lampert M, Haschke M, Drewe J, Krähenbühl S. Drug-related problems in hospitals: A review of the recent literature. Drug Saf 2007;30:379-407.
- Croskerry P, Sinclair D. Emergency medicine: A practice prone to error? CJEM 2001;3:271-6.
- World Health Organization. Rational use of drug report of the conference of experts 1987, 25-29 November 1985 Nairobi. Geneva: World Health Organization.
- World Health Organization. How to Investigate Drug Use in Health Facilities: selected Drug Use Indicators. Geneva: WHO; 1993. p. 1-87. WHO/DAP/93.1.
- Trostle J. Inappropriate distribution of medicines by professionals in developing countries. Soc Sci Med 1996;42:1117-20.
- Siddiqi S, Hamid S, Rafique G, Chaudhry SA, Ali N, Shahab S, et al. Prescription practices of public and private health care providers in Attock District of Pakistan. Int J Health Plann Manage 2002;17:23-40.
- Ojeniran M, Shouval R, Miskin IN, Moses AE, Shmueli A. Costs of appropriate and inappropriate use of antibiotics in the emergency department. Isr Med Assoc J 2010;12:742-6.
- Dhamija P, Bansal D, Srinivasan A, Bhalla A, Hota D, Chakrabarti A. Patterns of prescription drug use and incidence of drug-drug interactions in patients reporting to medical emergency. Fundam Clin Pharmacol 2013;27:231-7.
- Quick JD, Hogerzeil HV, Velasquez G, Rago L. Twenty-five years of essential medicines. Bull World Health Organ 2002;80:913-4.
- Cheekavolu C, Pathapati RM, Babasaheb Laxmansingh K, Saginela SK, Makineedi VP, Siddalingappa, et al. Evaluation of drug utilization patterns during initial treatment in the emergency room: A retroprospective pharmacoepidemiological study. ISRN Pharmacol 2011;2011:261585.
- Ruiz-López J, Calleja Hernández MA, Giménez Manzorro A, Sanjurjo Sáez M. Analysis of prescriptions given on discharge from the emergencies department. Economic impact. Farm Hosp 2009;33:104-10.
- Nixdorff N, Hustey FM, Brady AK, Vaji K, Leonard M, Messinger-Rapport BJ. Potentially inappropriate medications and adverse drug effects in elders in the ED. Am J Emerg Med 2008;26:697-700.
- Hogerzeil HV, Bimo, Ross-Degnan D, Laing RO, Ofori-Adjei D, Santoso B, et al. Field tests for rational drug use in twelve developing countries. Lancet 1993;342:1408-10.