Drug Utilization Pattern in Surgical Outpatient Department (OPD) at a Tertiary Care Hospital Situated in North Eastern Part of India-A Prospective Study
- *Corresponding Author:
- Devarsi Choudhury
Department of Pharmacology, Silchar Medical College and Hospital, Ghongoor, Assam, India.
E-mail: drdevarsi@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
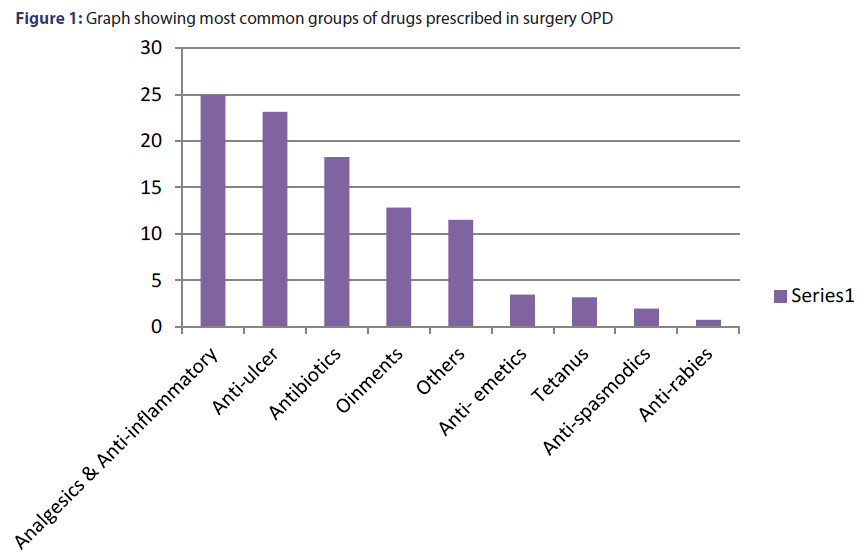
Objective: Prescription order is an important contract between the physician and patient. Regular inspection of prescriptions among surgery outpatients are hardly any in India. Therefore the present study was undertaken to study drug utilization pattern in the surgery OPD. Materials and Methods: A prospective, crosssectional study was conducted at a tertiary care center in Assam. A total of 920 prescriptions were randomly collected from the surgery OPD prescription papers existing from May 2016 to October 2016. The prescriptions were analyzed in the context of adherence to some of WHO core prescribing indicators. Results: Most number of cases arrived with complain of abdominal tenderness. The data was analyzed using WHO ‘prescribing indicators’. Average number of drugs per encounter was 3.05 ± 0.3. Drugs prescribed from National List Essential Medicine (NLEM) 2015 were 528 (57.4%). Encounters with an injection were 90 prescriptions (9.8%). The total no. of drugs prescribed by its generic name was 41.6% and the dugs given by its proprietary name was 58.4%. Most common group of drug prescribed was analgesics and antipyretics (24.96%), followed by antiulcers (23.13%) and antibiotics (18.25%). Most common drug prescribed was pantoprazole (11.55%), followed by diclofenac (10.24%) and amoxicillin and clavulanic acid (9.20%). Conclusion: This study provides a baseline data for carrying out further studies on prescribing pattern in a tertiary care unit. The pattern of prescription in terms of completeness and rationality was poor. There is an urgent need to improve the standards of drug prescription. On the basis of the finding of this study, adherence to essential drug list and generic prescription showed deviation from the standard recommended by WHO. This calls for sustained interventional strategies and periodic audit at all levels of health care. Injectable prescribing was not found to be a problem in this study.
Keywords
Prescription, OPD, antibiotics, drugs, generic
Introduction
Drug utilization study, as defined by the WHO, is a structured process which is used to assess the quality of drug therapy by engaging in the evaluation of data on drug prescribing, dispensing and patient use in a given health care environment, against predetermined, agreed upon criteria and standards, with special emphasis on the resulting medical, social, and economic consequences.[1] Drug utilization display prescribing performance of clinicians and assist in improving it.[2] Improper use of drugs symbolizes a potential peril to patients and an unnecessary expense.[3] Hence Drug Utilization Reviews (DURs) are very useful for discovering high cost drugs, which are of economic importance. Moreover, in India, Figures of drug usage pattern are not satisfactory. There is shortage of data on prescription pattern studies.[4]
Studies have to be done with proper monitoring of doses especially for the elderly and the children. Inter individual differences in age related pharmacokinetic and pharmacodynamic changes as well as co-morbid conditions should reflect while prescribing medicines in elderly population. Pharmacokinetic profiles of drugs changes considerably in the elderly because of reduced body water, renal and hepatic function and increased body fat. Multiple drug use and polypharmacy is extremely common in elderly divulging them to drug interactions and increased cost of therapy.[5] The drug administration in the pediatric population is also done cautiously as hazards of adverse effects are high. They have a small body surface area and also low renal function. Some drugs even impair the development of body parts. Unnecessary prescription of drugs in children has many pitfalls including amplification of consultation rates, wastage of resources, and exposing patients to adverse drug events. Studies have pointed out that children are prescribed drugs frequently, with an average number of drugs as high as 5.5.[6]
Setting principles and evaluating the quality of care through performance review must become a part of daily clinical exercise. Prescription pattern study is a component of medical audit which looks after monitoring, evaluation and necessary modifications in the prescribing practices of clinicians to accomplish rational and cost effective medical care.[7] Prescriptions should contain the essential drugs, which are easily available and almost free of cost at the government hospital pharmacies. WHO standards lay great stress on essential drugs. Essential drugs assure the healthcare needs of the majority of the population; as a result, they should be available at all times in sufficient amounts and in proper dosage forms, at a charge the community can afford.[8]
Most widespread irrational use of medicines is unwarranted use of antibiotics and injections. The expansion of resistant microbes will remain as a problem whenever antibiotics are used. The misuse and overuse of antibiotics have worsened the problem by adding up selection pressures favoring resistance.[9] Due to emerging resistance to combined antibiotics usage, most of the developing countries are troubled about the future availability of higher generation antibiotics, particularly the pediatric population, displaying resistance to mainstream antibiotics. Antibiotic use is very high in India varying from 24 to 67%.[10] Drug plays an inherent role in sustaining and reinstating health as well as to combat diseases. However, irrational use of drugs can lead to adverse drug reaction and negative socio-economic impact. To promote coherent use of drugs, international agencies like the World Health organization (WHO) and the International Network for the rational use of drugs have emphasized treatment of diseases by essential drugs, prescribed by their generic names.[6]
Implementation of the national list of essential medicines (NLEM) list for obtaining and supply of medicines, especially in public sector healthcare structure, has resulted in progress of availability of medicines, cost saving and more rational use of drug.[11] WHO prescribing indicators lays down fundamental rules for prescribing drugs. The hospital authority and the physicians must ensure that these are followed on a regular basis.
In surgery department, it is indispensable to supervise the use of drugs, taking consideration of the fact that parenteral administration of drugs like tetanus and anti- rabies vaccination takes place. Also, monitoring of drug availability is very essential in a developing country like ours. No studies were present on systematic audit of prescriptions among surgical outpatients in North Eastern part of India; hence, we took this study for highlighting the drug utilization followed in the surgery outpatient department (OPD) of the North-Eastern States of India. This hospital in our study is operational under the state government and as it serves as a major referral unit covering the major districts of Assam, there is an enormous rush of patients in the surgery OPD. As a result, elective operative cases are done at least 1 month after the diagnosis. This leads to conservative management of the patients with proper check up for a minimum period of one month. They are then specified with the date of the operative procedure. The emergency cases are operated as soon as possible with appropriate preparation at the operative theatres. The objectives of the study were the following:
• Prevalence outline of the diseases and demographic pattern at the surgery OPD.
• Analyze the prescriptions using the WHO prescribing indicators.
• Achieve information on the prescribing patterns of drugs in the surgery OPD.
• Analyze the patterns of drug use using the NLEM.[12]
• Obtain information regarding fixed drug composition (FDC) and investigations given.
Materials and Methods
The study was approved by the Ethics Research Committee. A cross sectional prospective study was conducted in surgery OPD of our hospital at Assam. As per WHO recommendations, it has been suggested that at least 600 encounters should be included in a crosssectional survey with a greater number if possible. Therefore, we collected nine hundred and twenty (920) prescriptions (average daily OPD attendance) randomly over a period of 6 months and were recorded over a WHO Prescribing Indicator Form. The data was then analyzed to find out the prescribing pattern in the hospital using the WHO prescribing indicators. WHO Prescribing Indicators: Average number of drugs per encounter, percentage of drugs prescribed by generic name, percentage of encounters with an antibiotic, antispasmodics, analgesics etc prescribed, percentage of encounters with an injection prescribed and percentage of drugs prescribed from essential drugs list or formulary. Data were entered and analyzed using Microsoft Excel 2007.
Results
Prevalence
Maximum cases were seen with the trouble of abdominal tenderness (23.3%) [Table 1]. They were sent for further investigations. Further investigations reveal most of these cases as appendicitis, cholecystitis, cholelithiasis, hemanigiomas, chroanic gastric ulcers, appendicitis, pancreatitis, liver cirrhosis, carcinoma of the intestines etc. Follow up cases (9.2%) consisted post-operative cases and the patients which are being prepared for elective surgery. Burns with <20% body surface area involvement are managed at this centre. It accounted 4% of the total cases during the study period. The cases we identified during this study period are: burns, follow up cases, fistula in ano, piles, appendicitis, burning micturition with fever, boils, pus, soft tissue injury, burns, road traffic accidents, hernia, parotid swellings, carcinoma breast, fibroadenoma, benign breast diseases, chest trauma, varicose veins, varicocele, hydrocele, cellulitis, boils.
| S No | Diagnosis | Total | Male | Female | Maximum no of cases seen in the age groups |
|---|---|---|---|---|---|
| 1 | Abdominal tenderness | 23.3 | 12.2 | 11.1 | 10-20 years |
| 2 | Follow up cases | 9.2 | 4.5 | 4.7 | 30-40 years |
| 3 | Benign breast disease | 11.9 | 1.8 | 10.1 | 20-30 years |
| 4 | Road traffic accidents | 8.7 | 5.4 | 3.3 | 20-30 years |
| 5 | Soft tissue infection & boils | 7 | 5 | 2 | 10-20 years |
| 6 | Dyspepsia | 3.5 | 2.2 | 1.3 | 30-40 years |
| 7 | Direct inguinal hernia | 4.8 | 3.6 | 1.2 | ≥ 50 years |
| 8 | Flatulence | 3.6 | 2.5 | 1.1 | 30- 40 years |
| 9 | Indirect inguinal hernia | 3.4 | 2.4 | 1 | 10-20 years |
| 10 | Burns (except deep burns) | 4 | 1.4 | 2.6 | 20- 30 years |
| 11 | Gastric ulcer | 2.1 | 1.5 | 0.6 | 30- 40 years |
| 12 | Neck swelling | 3.2 | 1.5 | 1.7 | 40- 50 years |
| 13 | Urinary tract infection | 2.7 | 1.1 | 1.6 | 20-30 years |
| 14 | Gastric ulcer | 1.2 | 0.9 | 0.3 | 20-30 years |
| 15 | Phimosis & circumcision | 3.4 | 3.4 | 0 | 0-10 years |
| 16 | Pancreatitis | 1.4 | 1.2 | 0.2 | 40-50 years |
| 17 | Fistula in ano | 1.3 | 1 | 0.3 | 30- 40 years |
| 18 | Carcinoma breast | 1.2 | 0 | 1.2 | 30- 40 years |
| 19 | Liver cirrhosis | 1.2 | 1.1 | 0.1 | 40-50 years |
| 20 | Varicose veins | 0.9 | 0.2 | 0.2 | 40- 50 years |
| 21 | Fistula in ano | 1.6 | 1.2 | 0.4 | 20- 30 years |
| 22 | Hydrocele | 0.2 | 0.2 | 0 | 20- 30 years |
| 23 | Carcinoma stomach & intestinal tract | 0.2 | 0.2 | 0 | 30-40 years |
| Total | 100 |
Table 1: Diagnosis pattern (%) in surgery OPD
In the age group of 0-10 yrs, highest cases were recorded with the diagnosis of phimosis. Those within the age group of 10- 20 years complained mostly of abdominal tenderness. In both the age groups of 20-30 years and 30-40 years, highest cases recorded among females were benign breast disease and cholelithiasis among the males. In the age group of 40-50 years, direct hernia was seen mostly among the males and piles among the females. For age group of ≥ 50 years, diagnosis of piles was common in females, whereas the male category topped the list with the incidence of direct hernia.
The following cases were referred to a higher centre attached with it, where specialized units like urology, plastic surgery, neurology etc are present: Deep burns, liver hemangioma on CT scan findings, burn contractures, and babies <1 year of age requiring operative procedures, severe head injury with CT scan findings and urology cases. Malignant cases requiring chemotherapy and radiotherapy are referred to the cancer institute. The cases diagnosed as road traffic accidents and requiring dressings are sent to the casualty department of our hospital. Proper management takes place here where the below poverty patients are provided with free investigations on producing suitable documents.
Demographic indicators
The male patients were higher in number than female patients (M 55%: F 45%). This male: female ratio difference (1.22) possibly is seen as women are dependent on the males to take them to hospital in rural India. This ratio speaks that women should be educated regarding the essential needs of healthcare and the facilities being provided at the government hospitals.
WHO core prescribing indicators
A total of 2805 drugs were prescribed on 920 prescriptions. This gave an average of 3.05 ± 0.30 (Mean ± Standard Deviation) drugs per encounter, with 528 (57.4%) of drugs from National List Essential Medicine (NLEM) 2015.[12] The percentage of encounters with an injection was 90 (9.8%). The total no. of drugs prescribed by its generic name was 41.6% and the dugs given by its proprietary name was 58.4% [Table 2]. It was seen that most of the drugs were given of different brands and also, same drug of different brands.
| Total number of prescriptions | 920 |
|---|---|
| Total number of drugs used | 2805 |
| Average number of drugs used per prescription | 3.05 ± 0.30 |
| Average number of drugs prescribed by its generic name | 41.6% |
| Average number of drugs prescribed by its proprietary (Brand) name | 58.4% |
| Average number of drugs prescribed from National List Essential Medicine (NLEM) 2015 | 57.4% |
| Polypharmacy | 62.4% |
| Percentage of prescriptions with injectables | 9.8% |
| Percentage of prescriptions where frequency of administration is not mentioned | 2.1% |
| Percentage of prescriptions where duration of drug therapy is not mentioned | 3.2% |
| Percentage of prescriptions where diagnosis was not mentioned | 11.6% |
| Percentage of prescriptions where signature of the physician was not present | 2% |
| Percentage of prescriptions where sex was not mentioned | 1.1% |
| Percentage of patients from urban and rural area | 66% and 34% |
Table 2: Assessment of who core prescribing indicators
Drug use pattern
Maximum number of antibiotics was prescribed for soft tissue infection (STI). Among the antibiotics, amoxicillin and clavulanic acid (9.2%) was most commonly prescribed, followed by cefixime (2.38%), amoxicillin (1.43%), tinidazole (2.2%) and cefpodoxime (1.02%) [Table 3]. Among analgesics and antipyretics, Diclofenac (10.24%) was mostly prescribed. Combination drugs diclofenac+paracetamol were found in use (3.65%). It was followed by aceclofenac (2.80%) and ibuprofen (2.07%). A higher use of anti-inflammatory drugs like serratiopeptidase (2.33%) and enzymes like trypsin and chymotrypsin (3.12%) was also revealed in our study. Figure 1 highlight the different groups of drugs prescribed in descending order.
| Antibiotics | Percentage (%) |
|---|---|
| Amoxicillin and Clavulanic Acid | 9.20 |
| Cefixime | 2.38 |
| Amoxicillin | 1.43 |
| Cefpodoxime | 1.02 |
| Levofloxacin | 0.8 |
| Ofloxacin+Ornidazole | 0.08 |
| Norfloxacin | 0.2 |
| Tinidazole | 2.2 |
| Ofloxacin | 0.32 |
| Azithromycin | 0.26 |
| Bacitracin | 0.16 |
| Clarithromycin | 0.2 |
Table 3: Percentage distribution of the antibiotics prescribed in the surgery OPD
Pantoprazole was the most commonly prescribed medication (11.55%) among the gastro protective drugs which was much higher than the other similar drugs like rabeprazole (5.25%) and omeprazole (3.34%). Anti-emetics like ondansetron (1.4%) and anti-spasmodics like dicyclomine (2.4) in addition were prescribed. Laxatives were used in 0.40% of the cases.
Multivitamins were found in use to the extent of 11.2%. Anti-bacterial ointments like mupirocin (1.67%), bacitracin (1.57%) and fusidic acid (0.03%) were prescribed. Burn cases were managed by the ointment Silver X (1.87%). The ointment with the brand name Thank God (1.83%) was used on regular basis.
FDC
Out of the total 2805 formulations prescribed, 481 (17.13%) were FDCs. FDCs were most commonly prescribed in the age group of 30- 40 years age group [Table 4].
| Drugs | Percentage (%) |
|---|---|
| Diclofenac+paracetamol | 3.65 |
| Diclofenac+paracetamol+serratipeptidase | 0.40 |
| Ofloxacin+ornidazole | 0.08 |
| Amoxicillin+tinidazole/clarithromycin+omeprazole | 1.8 |
| Multivitamins | 11.2 |
Table 4: Frequently prescribed fdcs in surgery OPD
Investigations given
Following were the necessary investigations set down for the operative cases: routine investigation of blood, total leucocyte count, differential leucocyte count, liver fuction test, kidney function test, ECG, HCV, HbsAg, random blood sugar, fasting blood sugar, HIV 1 and 2, platelet count, hemoglobin%, bleeding time, clotting time, prothrombin time with INR, erythrocyte sedimentation rate, TSH etc. Details of previous history of operative procedures, whether diabetic, hypertensive, anemic, family history, economic background etc. were taken into account. Emergency cases were directly admitted from OPD and necessary treatment was followed.
Discussion
In a study conducted at Oman, the average number of drugs per prescription was 2.3 ± 1.5, and it was almost similar in all age groups. [6] In the study by Banerjee et al.[13] average number of drugs per prescription in a primary health center by the interns was 2.58, while the number of drugs per prescription varied from 1 to 7. The study by Barot et al. even reported that number of drugs prescribed per patient was 9.99 ± 2.55 (Mean ± standard deviation).[14] This study was carried in the emergency department so we can have a diverse result with the rest of the studies. In an average, the number of drugs prescribed by urban and rural area General practitioners was nearly 5 and 4, respectively. It was a community based descriptive study was conducted in a randomly selected urban and rural area of Tamil Nadu. [9] Our study recorded 3.05 ± 0.30 drugs per prescription. This finding is divergent with the above-mentioned studies.
Balushi et al. reported that only 15% of the drugs were prescribed intravenously in their hospital.[6] The interns prescribed injectables in 89 prescriptions (4.49%).[13] Rehana et al. reported that injections containing antibiotics was frequent as evidenced by a mean of 2.12 injections per prescription at a health institute in Nepal.[15] Gopalakrishnan et al. stated that nearly 80% of the urban and rural GPs were prescribing at least one injection.[9] Our study showed that percentage of prescriptions with injectables was 9.8%. This is a suitable finding reflecting the fact that accidents and animal bites cases must receive the necessary vaccinations which are administered as injectables.
Al Balushi et al. confirmed that co-amoxiclav followed by azithromycin were the most common drugs prescribed from the antibiotics section. [6] Barot et al. mentioned ceftriaxone was the most commonly prescribed antibiotic in 51 (32.69%) patients.[14] In Eastern Nepal, the most frequently used antibiotics were cloxacillin (20.4%), ampicillin (19.8%) and metronidazole (15.6%). They even recorded the use of combinations of antibiotics, where ciprofloxacin plus metronidazole and crystalline penicillin plus chloramphenicol administration was highest.[15] Gopalakrishnan et al. revealed among the antibiotics prescribed, capsule amoxicillin (49.2%) and injection gentamicin (31.7%) were the most commonly prescribed in both urban and rural areas and co-trimoxazole was the least prescribed antibiotic (11.5%). [9] In another study, ciprofloxacin, metronidazole and penicillin G were most frequently prescribed while vancomycin, chloramphenicol and oxytetracycline were relatively least prescribed antibiotics.[16] Overall prescribing frequency in their hospital for penicillins and cephalosporins was 67.82%, quinolones 34.25%, aminoglycosides 31.83%, metronidazole 25.25%, tetracycline and chloramphenicol 4.84% and vancomycin 1.03%.[16] Our study sited that out of the total number of drugs, amoxicillin and clavulanic acid (9.2%) was most commonly prescribed, followed by cefixime (2.38%), amoxicillin (1.43%), tinidazole (2.2%) and cefpodoxime (1.02%). This was a parallel trend observed in different parts of the world.
Paracetamol was the most commonly prescribed drug in the study population at Oman, with a prevalence rate of nearly 13%, followed by salbutamol (8%), while ibuprofen was the most prescribed drug in those aged ≥ 12 years.[6] Analgesics were the most commonly prescribed drug by the interns (25.78%) followed by antibiotics, drugs used for gastrointestinal symptom (diarrhea/vomiting etc.) multivitamins, anti-malarial, antihistaminic, hematinics, etc.[13] The most frequently used drugs in the emergency department were 5-hydroxytryptamine3 (5-HT3) receptor antagonist ondansetron 135 (86.53%) and proton pump inhibitor (PPI) pantoprazole 133 (85.25%) followed by furosemide 68 (43.58%).[14] The study by Rehana et al. said that most frequently administered groups were antibiotics (42.8%), followed by analgesics and anti-inflammatory agents (13.1%), vitamins (7.3%), steroids (3.8%) and H-receptor blockers (3.0%).[14] Out of the 600 prescriptions by the urban and the rural GPs, it was observed that multivitamins were the most commonly prescribed drug followed by antibiotics, drugs used for gastro-intestinal tract diseases, analgesics, antihistamines, and antipyretics.[9] Kafle et al. stated analgesics and antibacterials share highest drug utilization groups.[17] Our study addressed that analgesics and anti-inflammatory drugs (24.96%) was most commonly used followed by the anti-ulcer drugs (23.13%) and the antibiotics (18.25%).
Al-Balushi observed that in the pediatric population, the frequency of drug administration was mentioned in 726 (95.52%) of the prescriptions, while the duration of therapy was recorded in 586 (77.1%) of them. A total of 688 (34.97%) drugs were prescribed by generic name while the percentage of drugs prescribed from EDL of India was 58.47%.[6] Barot PA et al. made an encouraging finding. They said about 88% of drugs were prescribed by brand name out of which 84.5% drugs belonged to NLEM India.[14] Rehana et al. mentioned the percentage of drugs prescribed by generic name was 29.3%.[15] In Tamil Nadu as mentioned by Gopalakrishnan S et al., nearly 71% of urban GPs were prescribing the drugs by generic name, but only 52% of the rural GPs did that. It is also observed that 34.7% of rural and 40% of the urban GPs prescribed drugs from the essential drug list.[9] Our study pointed that 528 (57.4%) of drugs were prescribed from NLEM 2015. The total no. of drugs prescribed by its generic name was 41.6% and the dugs given by its proprietary name was 58.4%.
Barot et al. said that FDCs comprised 8% of total drugs.[14] Rehana et al. found that of the drugs prescribed, 5.4% were fixed dose combinations. [15] Balat et al. had done a study on the pattern of FDCs in Ahmedabad, India. The FDCs prescribed there 941 (80.3%) with an average of 1.41 ± 1.04 (mean ± SD) per prescription.[18] Pramila et al. found a rise in the use of FDCs (75.49%). The commonly used FDCs were NSAIDS with decongestants (53.24%), diclofenac and paracetamol (20.77%), and ibuprofen with paracetamol (15.58%). These figures seem quite suitable for an ENT OPD.[19] The study at a Dermatology OPD alleged that FDCs prescribed were 11.9%.[20] We found in our study that 17.13% of the drugs specified were FDCs.
The act of polypharmacy is described as prescribing more than or equal to three drugs per prescription. Gopalakrishnan et al. in reported that polypharmacy in both urban and rural areas of Tamil Nadu were high.[9] Narwane et al. revealed that polypharmacy found in the prescriptions were 58%.[20] Polypharmacy is growing because of not only co-morbid conditions but also due to increased awareness about drugs, literate elders or care takers and pressure on the physicians to prescribe a drug for each indication. In another study, polypharmacy was observed in 88.67% cases. 5-8 drugs were prescribed for most patients (46.22%), followed by >8 drugs (42.45%).[6] In the psychiatry OPD, polypharmacy was inscribed in 47.12% of the prescriptions.[21] A recent report published by the King’s Fund in the UK has promoted the term “appropriate polypharmacy” described as prescribing for an individual with complex or multiple conditions where medicine use has been optimized and prescribing is in accordance with best evidence, rather than existing thresholds that define polypharmacy based on the number of prescribed medications. The concept of “appropriate polypharmacy” recognizes that patients can benefit from multiple medications provided that prescribing is evidence based and reflects patients’ clinical needs.[15]
Conclusion
The percentage of drugs prescribed from the essential medicine list was found to be low and the average number of drugs per prescription was found to be high. This study reveals that abdominal tenderness presented as most number of cases in the surgery OPD department. Polypharmacy was prevalent which brought in the problems of drug interactions. Our study had limitations too. Efforts must be done to conduct studies throughout the year as seasonal variation of diseases is there. Also, comparative assessment of prescriptions with other clinical departments must be done. Educational sessions, especially for the junior doctors on the correct method of writing prescriptions should be organized.
Conflicts of interest
None
Financial support and sponsorship
Nil
References
- Jimoh AO, Etuk EU, Sani Z, Shuaibu HA. The pattern of antibiotic use in a family medicine department of a tertiary hospital in Sokoto, North Western Nigeria. J Clin Diagn Res 2011;5:566-9.
- Memon A, Patel K. Drug use pattern of antidepressant agents in psychiatric patients – A prospective study. J Med Sci 2013;2:33-6.
- Introduction to Drug Utilization Research by World Health Organization. Available from: http://www.whocc.no/filearchive/publications/drug_utilization_research.pdf
- Assen M, Muhammed OS. Assessment of prescribing pattern in Borumeda hospital North East Ethiopia. Int J Pharm Sci Res 2015;6:1214-9.
- Veena DR, Padma L, Patil S. Drug prescribing pattern in elderly patients in a teaching hospital. J Dental Med Sci 2012;1:39-42.
- Al-Balushi KA, Al-Sawafi F, Al-Ghafri F, Al-Zakwani I. Drug utilization pattern in an Omani pediatric population. Search Results. J Basic Clin Pharm 2013;4:68-72.
- WHO Regional Publications. Studies in drug utilization. European Series No. 8. Copenhagen: WHO Regional publications, 1979.
- WHO Expert Committee. The use of essential drugs. World Health Organ Technical Report Series 2000;895:1-61.
- Gopalakrishnan S, Ganeshkumar P, Katta A. Assessment of prescribing practices among urban and rural general practitioners in Tamil Nadu. Indian J Pharmacol 2013;45:252-7.
- Ahmad A. Study the Prescription Pattern of Antibiotics in the Medicine Department in a Teaching Hospital: A Descriptive Study. Int J Toxicol Pharmacol Res 2014;6:43-6.
- Tripathi KD. Essential Drugs (medicines) concept. Essentials of Medical Pharmacology. 6th edn. New Delhi: Jaypee Brothers;2008;5-6.
- National List of Essential Medicines of India 2015;1-117. Available at http://cdsco.nic.in/WriteReadData/NLEM-2015/NLEM,%202015.pdf (Last accessed on 11/29/2016).
- Banerjee I, Bhadury T. Prescribing pattern of interns in a primary health center in India. J Basic Clin Pharm 2014;5:40-3.
- Barot PA, Malhotra SD, Rana DA, Patel VJ, Patel KP. Drug utilization in emergency medicine department at a tertiary care teaching hospital: A prospective study. J Basic Clin Pharm 2013;4:78-81.
- Rehana HS, Nagarani MA, Rehan M. A study on the drug prescribing pattern and use of antimicrobial agents at a tertiary care teaching hospital in Eastern Nepal. Indian J Pharmacol 1998;30:175-80.
- Gupta N, Sharma D, Garg SK, Bhargava VK Auditing of prescriptions to study utilization of antimicrobials in a tertiary hospital. Indian J Pharmacol 1997;29:411-5.
- Kafle KK, Rajbhandari SM, Srivastava K, Regmi S. Drug prescribing in out-patient departments in teaching hospital in Nepal. Indian J Pharmacol 1991;23: 219-21.
- Balat JD, Gandhi AM, Patel PP, Dikshit RK. A study of use of fixed dose combinations in Ahmedabad, India. Indian J Pharmacol 2014;46:503-9.
- Yadav P, Kanase V, Lacchiramka P, Jain S. Drug utilization trends in ENT outpatient department in a teaching hospital. Int J Pharma Bio Sci 2010;1:153-60.
- Narwane SP, Patel TC, Shetty YC, Chikhalkar SB. Drug Utilization and Cost Analysis for Common Skin Diseases in Dermatology OPD of an Indian Tertiary Care Hospital - A Prescription Survey. Br J Pharm Res 2011;1:9-18.
- Karak Hati S, Sil S, Dalui SK, Dutta SK, Biswas S. Polypharmacy dominated prescribing pattern of antipsychotic drugs in a tertiary care hospital. World J Pharmacol Pharm Sci 2016;5:1045-55.