Analysis of Prescribing Pattern and Techniques of Switching Over of Antipsychotics in Outpatients of a Tertiary Care Hospital in Delhi: A Prospective, Observational Study
- *Corresponding Author:
- Dr. Shankar Kumar
Department of Pharmacology, Maulana Azad Medical College, University of Delhi, New Delhi.
E-mail: skumar071988@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Context: Drug utilization study, prescribing practices, switchovers. Aims: The present study aims to analyze antipsychotic prescriptions, assess whether they conform to WHO core prescribing indicators and identify types and reasons behind switching over from one antipsychotic to another. Settings and Design: The present study, prospective and observational in design, was conducted in the psychiatry outpatients department of a tertiary care hospital in Delhi for 1 year. Methods and Material: A total of 224 patients enrolled were followed up for a period of 90 days. WHO core prescribing indicators were assessed. Technique of switching over from one antipsychotic to another was monitored. Statistical analysis used: The data was entered and analysed using statistical software SPSS 17.0. The demographic data was presented as Mean +/- Standard deviation. The WHO core drug prescribing indicators were expressed as percentages. For all statistical analysis, a p value of <0.05 was considered significant at a confidence interval of 95%. Results: A total of 293 antipsychotics were prescribed over the 90 day study period, of which 88.7% belonged to atypical class. Antipsychotics were used for off label indications 18 times. The use of anticholinergics was 18.8% against 32.9% antipsychotic usage. Polypharmacy was reported in 14.17% cases. We report 52 patients who switched over from one antipsychotic to another once during the study period while 3 patients switched over twice, thus amounting to total of 58 switches. Conclusions: Polypharmacy and off label prescribing needs to be carefully monitored and practices like prescribing from essential medicines list and by generic name need to be encouraged. Early switching over could be related to adverse effect while switch over later on in therapy could raise questions on efficacy of the drug
Keywords
Antipsychotics, prescribing pattern, polypharmacy, switch, drug utilization
Introduction
Over the past decades, innumerable utilization studies using WHO drug use indicators have been carried out in different health care settings in India. However, drug utilization studies involving drug use indicators are lacking for psychiatry patients. Psychotropic, psychoactive or psychotherapeutic drugs are the medication used for pharmacological treatment of mental disorders. These have been classified traditionally as antipsychotics, antidepressants, mood stabilizers and antianxiety or sedative hypnotics.[1]
Few studies have been done in India, which have evaluated the prescription pattern of antipsychotic medications. Prescription pattern of all hospitalized patients with diagnosis of schizophrenia was studied and risperidone (56.17%) was found to be the most commonly prescribed antipsychotic followed by olanzapine (21.34%) and quetiapine (3.93%).[2] Typical antipsychotics were used in 15.73% of the cases and polypharmacy (use of more than one antipsychotic) was observed in 9% of the cases.[2] In another study, olanzapine (64%) was found to be the most commonly prescribed antipsychotic followed by risperidone (48%) and flupenthixol injection (17%) conducted in outpatients psychiatry clinic.[3] A retrospective cohort analysis of drug prescriptions in schizophrenia diagnosed patients was done using data from a German health insurance fund. Out of a total of 56,692 prescriptions, olanzapine (26.6%) was the most frequently prescribed followed by clozapine (21.3%).[4] In a retrospective audit of 1591 prescriptions at a psychiatric hospital in Bahrain, atypical antipsychotics (67.7%) were found to be most commonly prescribed and risperidone was the most frequent drug in this class.[5] A preliminary survey of 168 psychiatrists in India was done and based on the response to the questionnaire, they concluded that risperidone, olanzapine and haloperidol were among the most commonly prescribed antipsychotics.[6] Atypical antipsychotics (77%) were most commonly prescribed to 116 patients at a Mumbai hospital who had first episode of schizophrenia and risperidone (20.8%) followed by quetiapine (19.8%) were mostly used.[7] A cross sectional study was carried out in a psychiatry outpatients department at Burdwan Medical College, Kolkata to describe the prescribing patterns of antipsychotics. Out of 510 prescriptions, atypical antipsychotics were most commonly prescribed and olanzapine (77.06%) was clearly the most frequently used antipsychotic.[8] Drug utilization studies are of great relevance in the context of a developing country like India with lesser resources and in healthcare systems providing medicines from the essential medicines list. The purpose of studying prescribing patterns of antipsychotics is to ensure and promote rational use of such drugs to enhance therapeutic efficacy, provide feedback to prescribers about the pattern, and decrease the incidence of adverse drug reactions.[9]
Previous studies of the prescription patterns of psychotropic medications in patients with schizophrenia have highlighted a high rate of antipsychotic polypharmacy, but data in Asia are sparse. A study conducted in Singapore examined the prevalence of antipsychotic[10] polypharmacy in 2399 patients with schizophrenia across six south east Asian countries (China, Hong Kong, Japan, Korea, Singapore, and Taiwan) and compared the differences between patients receiving one vs. those receiving more than one antipsychotic. Antipsychotic polypharmacy was found in 45.7% (n=1097) of the patients with wide intercountry variations.10 Polypharmacy was associated with male gender, advanced age, psychiatric hospital setting, anticholinergic use and less use of an atypical antipsychotic drug (OR 0.83, 95% CI 0.71, 0.98, p<0.05).10 In another study conducted in Nagpur, off label use of psychotropics was found in 53 of 515 prescriptions (10.29%). 61.5% of the prescriptions had polypharmacy. Incidences of polypharmacy noted in some other studies were 41.9% and 100%.[11,12] Anticholinergics were concomitantly used with typical as well as atypical antipsychotics. This could be due to unawareness of prescribers to advantages of atypical over typical antipsychotics or false claims of low incidence of extrapyramidal side effects with atypical antipsychotics by marketing people. Prescribers’ explanation to this practice is to prevent occurrence of adverse drug reaction to typical antipsychotic. Atypical antipsychotic co-prescription with typical antipsychotic is likely to nullify this potential benefit.[13] Such use is deemed inappropriate. Typical and atypical antipsychotics together had shown to increase frequency of extrapyramidal side effects and early death.[14,15]
Antipsychotic drugs can be used to help treat a wide variety of psychiatric disorders. However, specific antipsychotic drugs for any particular patient may need to be changed for a number of different reasons, including a lack of therapeutic efficacy and/ or intolerance to medication side effects. Drug switching may occur through a limited number of established patterns. A study conducted in Canada observed patients for one year prior to and during admission to the hospital, and of the 139 patients enrolled, a total of 31 switched antipsychotic drugs. The frequency of switching increased closer to the time of admission, and the proportional rate of switching was even higher during hospital stay. The most common switch was from risperidone to quetiapine. The analysis identified three main patterns of drug switching, all occurring with similar frequency: titrated drug switches, abrupt drug switches and concurrent drug administration. However, the study could not indicate whether any specific manner of drug switching predominates.[16]
Off-label drug prescribing is very common in Psychiatry. US-Food and Drug Administration has defined off-label drug as “use of drugs for the indication, dosage form, regimen, patient, or other use constraint not mentioned in the approved labelling.” A one year long, prospective, cross sectional study was conducted in Gujarat to evaluate off-label drug use in patients attending Outpatient Department of Psychiatry.[17] A total of 980 drugs were prescribed out of which 387 (39.5%) were off-label. Of 250 patients, 198 (79.2%) received at least one off-label drug.29 Inappropriate indication was the most common category of off-label use. Off label use of atypical antipsychotics was seen in 14 (5.6%) patients only.
In the study conducted in Nagpur, olanzapine had been used off label for mental retardation (n=4), bipolar disorder (n=6), organic delirium state (n=1), depression (n=1), insomnia (n=1), organic brain syndrome (n=1), mania (n=2), post ictal confusion (n=1), dementia (n=6), seizure disorder (n=2), delirium (n=1) and obsessive compulsive disorder (n=1).[18] Prescribing in such a way needs a careful and documented analysis of the potential risks and benefits.
Aims and objectives
To describe the prescribing pattern of antipsychotics in outpatients of a tertiary care hospital in Delhi.
To report the technique of switching over and determine if any temporal relationship exists.
Subjects and Methods
Study settings
The study was conducted in the Department of Pharmacology, Maulana Azad Medical College and Department of Psychiatry at Govind Ballabh Pant (G.B. Pant) Hospital, New Delhi. G.B. Pant Hospital is a 600 bedded super speciality hospital which provides health services to patients form Delhi and neighbouring regions. The Outpatients Department (OPD) of Psychiatry provides services from 9.00 A.M till 1.00 P.M. from Monday to Saturday.
Study design
The study was designed as a hospital based prospective and observational study.
Study Population: The study population were outpatients visiting Psychiatry Department of G.B. Pant Hospital.
Study duration: The study was conducted for a period of one year (January 2014- January 2015). The patients enrolled were followed up for a period of 3 months (90 days).
Ethical clearance
The study was conducted after Institute Ethics Committee approval.
Inclusion criteria
All patients who were 18 years and above, of either sex, who had been newly diagnosed and prescribed one or more antipsychotic drugs were included in the study. The study included only outpatients visiting the hospital.
Exclusion Criteria: Patients excluded from the study were as follows- Inpatients, Patients on substance abuse.
Informed consent
Patients and/or their attendants were made to understand the purpose, their rights, and the procedure of the study with the help of patient information sheet and written informed consent prepared in Hindi and English. Left thumb impression fingerprint was taken in the presence of an appropriate witness for illiterate patients.
Sample size estimation
A total of 224 patients were enrolled. This was calculated based on data obtained from a study by Ghosh et al. using α-5% , power- 80%, and acceptable error-10%.8
Data collection
Patients were enrolled after written informed consent and as per the inclusion criteria. Prescriptions of patients visiting outpatients department (OPD) of G.B. Pant Hospital, New Delhi were collected on the first day of visit and analysed for patterns of antipsychotic drug prescribing. Patients were included if they were prescribed atleast one antipsychotic drug irrespective of diagnoses. Any change in prescribed antipsychotic, i.e., switch over, was recorded but the prescription of individual patient was analysed on the whole and considered as a single case record.[19] The World Health Organisation (WHO) prescribing drug indicators were used for analyses which are as follows :-
1. Average number of drugs per encounter-calculated by dividing the total number of drugs prescribed, by the number of encounters surveyed.
2. Percentage of drugs prescribed by generic name-calculated by dividing the number of drugs prescribed by generic name, by the total number of drugs prescribed, and multiplied by 100.
3. Percentage of encounters with an injection prescribed–calculated by dividing the number of encounters wherein an injection was prescribed, by the total number of encounters surveyed, and multiplied by 100.
4. Percentage of drugs prescribed from Essential Drugs List (EDL) or formulary-calculated by dividing the number of drugs prescribed from the EDL or formulary, by the total number of drugs prescribed, and multiplied by 100.
The patients were followed for 3 months or 90 days both telephonically as well as during subsequent visits to the outpatients department. In the outpatients department, patients are followed up every 2 weeks for medication refills as well. These approaches were undertaken to decrease the bias arising due to loss to follow up. At the end of the study period, i.e., 90 days, the following were noted.[20-22]
Prescription analysis to note for changes, if any. Changes in prescription noted were ‘switch overs’ from one drug group to another, or prescribing from within the same group, or ‘add- on’ drugs to the existing prescription, either due to inadequate response or adverse drug reaction with the medication. “Switches” were defined as when one antipsychotic was terminated and a different antipsychotic was started within at least 3 weeks, or if the two antipsychotic prescriptions overlapped with a titration down (eventually ending in termination) within 3 weeks. Switches were classified into one of four categories, based on previously defined approaches:
(i) Titrated - At least one drug was tapered,
(ii) Immediate - First drug was terminated and the second drug started abruptly with no overlap or tapering,
(iii) Gap - Gap of less than 3 weeks between antipsychotic prescriptions, and
(iv) Overlapping - Both the initial and the new antipsychotic were given concurrently for some period of less than three weeks ending in a termination of the first antipsychotic with no titration down.[16]
Other indicators that were used are as follows-
• Percentage of fixed dose combinations prescribed.
• Percentage of patients receiving more than one antipsychotic.
• Percentage of polypharmacy (prescribing 4 or more drugs)
• Percentage of patients receiving other psychotropic medications like antidepressants, anxiolytics, sedative hypnotics,etc. and also non psychotropic medications and nutraceuticals.
Statistical analysis
The data was entered and analysed using statistical software SPSS 17.0. The demographic data was presented as Mean +/- Standard deviation. The WHO core drug prescribing indicators were expressed as percentages. The patients who were lost to follow up were not included in the final analysis. Only those patients who completed the 90 day study period were included to get an accurate measurement of the frequency of switching over. For all statistical analysis, a p value of <0.05 was considered significant at a confidence interval of 95%.
Results
Majority of the patients belonged to age group of 31-40 years (31.4%), followed by age group of 18-30 years (28.6%) and 41-50 years (27.5%). Other age groups of 51-60 years (7.3%), 61-70 years (3.1%) and >70 years (2.1%) constituted minority of the patients. Males constituted 52.7% (n=118) while females were 47.3% (n=106) of the total participants. In terms of marital status, as many as 59% patients were married while 32% patients were single/unmarried. A small fraction of patients were either widowed (7%) or divorced (2%). As many as 31% patients included in the study were illiterate and the same proportion had education level up till primary school (31%). Only 26% went to secondary school while 10% had had a graduation and only a meagre 2% were professional. Of the 224 patients included in the study, 53% were employed while 47% were unemployed. The patients in the study were almost equally distributed amongst those living in a nuclear family (49.7%) and those living in a joint family (50.3%).
Antipsychotic drug prescribing pattern
ICD-10 diagnoses of patients receiving antipsychotics
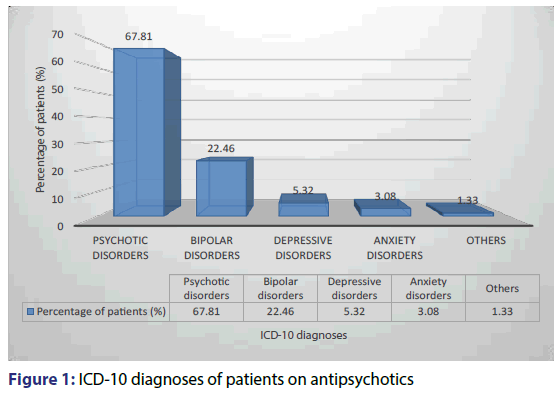
Psychotic disorders (67.81%) was the major diagnosis amongst the patients enrolled. This was followed by bipolar disorder (22.46%), depressive disorders (5.32%) anxiety disorders (3.08%) and other disorders in which antipsychotics were prescribed off label (1.33%) as shown in Figure 1.
Usage of antipsychotics
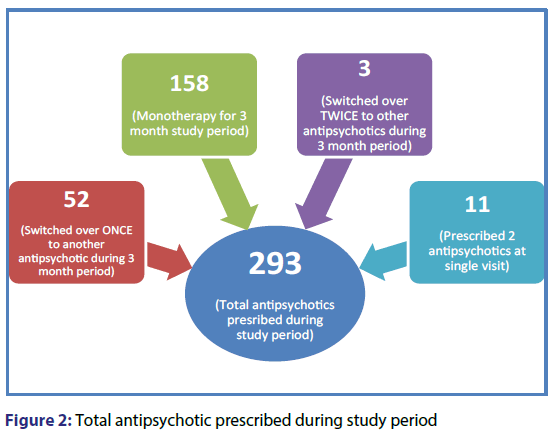
As shown in the Figure 2 below, 158 of the 224 patients enrolled in the study received monotherapy with a single antipsychotic throughout the 3 month period. 52 of the total 224 patients were switched over from one antipsychotic to another, hence their usage comes out to be 2 antipsychotic per patient during study period (total=104). It is to be noted here that while switching a simultaneous taper of one antipsychotic and initiation of second antipsychotic is a common occurrence. These patients are not the same as patients who are prescribed two antipsychotics by virtue of their diagnosis. Such patients are grouped separately as mentioned below. Three patients had 2 switch overs, and therefore were given total of 3 antipsychotics during the study period, and hence a total of 9 antipsychotics in this category. Eleven patients received 2 antipsychotics during a single visit due to the severity of diagnosis or otherwise, and hence amounting to 22 antipsychotics being prescribed in this category. Therefore, a total of 293 antipsychotics were prescribed or the number of times an antipsychotic was prescribed comes out to be 293. Atypical antipsychotics constituted 88.7% of the total number of times an antipsychotic was prescribed whereas typical antipsychotics were prescribed 11.3% of the times.
Percentage of number of times individual antipsychotic prescribed [n=293]
Risperidone had been most commonly prescribed antipsychotic (44.71%) followed by olanzapine (34.81%) and aripiprazole (7.12%). Other antipsychotics like clozapine (5.32%), quetiapine (2.95%), trifluoperazine (2.67%), haloperidol (2.5%), amisulpride (1.34%) and fluphenazine (0.45%) were prescribed in fewer patients.
Indication wise use of various antipsychotics
Table 1 below shows use of different antipsychotic agents in different diagnoses. Risperidone had been prescribed 131 times, mostly in psychotic disorders (n=79) and bipolar disorders (n=50). Likewise, aripiprazole had been used 21 times, clozapine 15 times, quetiapine and trifluoperazine both 8 times, while haloperidol, amisulpride and fluphenazine were used total of 12 times.
| Drug | Psychotic disorders [n=152] |
Bipolar disorders [n=50] | Depressive disorders [n=12] | Anxiety disorders [n=7] | Others [n=3] |
|---|---|---|---|---|---|
| Risperidone [n=131] | 79 | 39 | 6 | 4 | 3 |
| Olanzapine [n=102] | 68 | 24 | 4 | 3 | 0 |
| Aripiprazole [n=21] | 18 | 0 | 3 | 0 | 0 |
| Clozapine [n=15] | 15 | 0 | 0 | 0 | 0 |
| Quetiapine [n=8] | 8 | 0 | 0 | 0 | 0 |
| Trifluoperazine [n=8] | 8 | 0 | 0 | 0 | 0 |
| Haloperidol [n=7] | 5 | 1 | 0 | 0 | 1 |
| Amisulpride [n=4] | 4 | 0 | 0 | 0 | 0 |
| Fluphenazine [n=1] | 1 | 0 | 0 | 0 | 0 |
Table 1: Indication wise use of different antipsychotics
Number of drugs prescribed per patient per encounter
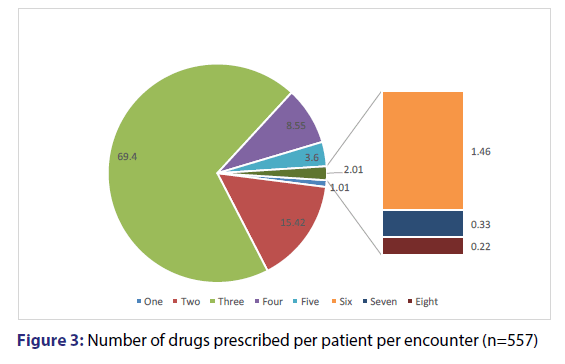
Total number of encounters with patients enrolled in the present study was 557. The number of drugs prescribed per patient per encounter was determined. As many as 69.4% patients had an average of 3 drugs per visit. 15.42% patients received average of 2 drugs during their visit, 8.55% received 4 drugs, 3.6% received 5 drugs, 1.01% received 1 drug, while 2.01% received more than 6 drugs per encounter [Figure 3].
WHO prescribing indicators
The WHO core prescribing indicators were evaluated. We noted an average of 3.12 (± 0.41) drugs per encounter. Only 16.22% of drugs were prescribed by generic name. Remaining were prescribed using brand names available in local pharmacies near the hospital. We report zero encounters wherein an antibiotic was prescribed. An injection of fluphenazine was prescribed to one patient (0.44%). Majority of the drugs (72.41%) were prescribed from the hospital Essential Medicines List [Table 2]. Other indicators noted were percentage of fixed dose combinations, patients who were prescribed more than one antipsychotic at a single visit. We found no usage of fixed dose combinations. Only 11 patients (4.91%) had been prescribed more than one antipsychotic at a single visit. These 11 patients were exclusive of those having titrated or overlapping switchovers.
| S.No | Indicators | Value |
|---|---|---|
| 1. | Average no. of drugs per encounter | 3.12 ± 0.41 |
| 2. | Percentage of drugs prescribed by generic name | 16.22 |
| 3. | Percentage of encounters with an antibiotic prescribed | 0 |
| 4. | Percentage of encounters with an injection prescribed | 0.44 |
| 5. | Percentage of drugs prescribed from Essential Medicine List | 72.41 |
Table 2: WHO Prescribing indicators
Concomitant medications used
Total of 224 case records were analysed, of which 636 psychotropic medications were prescribed, which included 293 antipsychotics (46% of total psychotropic drugs) and 343 other psychotropic agents (54% of total psychotropic drugs). These classes of psychotropic medications included sedative hypnotics (34.9%), mood stabilizers (11.16%) and antidepressants (7.86%). A record of other medications (n=252) besides psychotropic agents were also kept. These included centrally acting anticholinergics like trihexyphenidyl (n=167) and other nutraceuticals like vitamin complex combinations. Therefore, a total of 888 drugs, i.e., 636 psychotropic agents and 252 non psychotropic drugs and/or nutraceuticals, were prescribed.
Switch over and drug class
Table 3 below shows the antipsychotic agent that was switched over to some other antipsychotic agent due to various reasons. In our study, a total of 52 patients had to be switched over from one antipsychotic to another. Of these 3 patients had 2 switchovers during the study period of 3 months. Hence, the total number of switches were 58. Maximum switches reported were titrated (n=20, 34.48% of total switches), followed by gap (n=14, 24.13% of total switches), immediate (n=13, 22.41% of total switches) and overlapping (n=11, 18.96% of total switches) as shown below. Risperidone (n=18) and olanzapine (n=18) were switched maximally compared to other agents.
| Titrated switch (% of total switches) |
Immediate switch (% of total switches) |
Gap switch (% of total switches) |
Overlapping switch (% of total switches) |
|
|---|---|---|---|---|
| Risperidone | 6 (10.34) | 1 (1.72) | 5 (8.62) | 6 (10.34) |
| Olanzapine | 5 (8.62) | 4 (6.89) | 5 (8.62) | 4 (6.89) |
| Aripiprazole | 2 (3.44) | 0 (0) | 0 (0) | 0 (0) |
| Clozapine | 3 (5.17) | 4 (6.89) | 1 (1.72) | 1 (1.72) |
| Quetiapine | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Trifluoperazine | 2 (3.44) | 1 (1.72) | 2 (3.44) | 0 (0) |
| Haloperidol | 2 (3.44) | 2 (3.44) | 1 (1.72) | 0 (0) |
| Amisulpride | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Fluphenazine | 0 (0) | 1 (1.72) | 0 (0) | 0 (0) |
| Total (n=58) | 20 (34.48) | 13 (22.41) | 14 (24.13) | 11 (18.96) |
Table 3: Switch over type and associated antipsychotic
Distribution and type of switch between antipsychotics over 12 week period
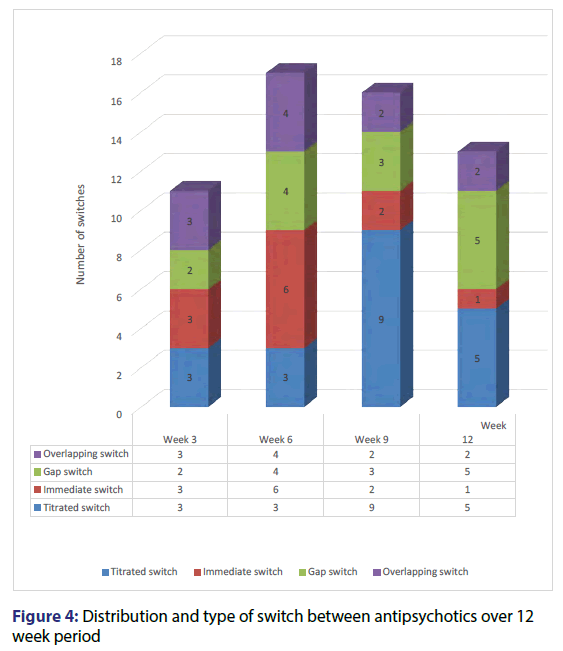
Figure 4 below shows the study period of 3 months or 90 days divided into 3 week periods. We noted the number and type of switches as and when they occurred. Most of the switches occurred with similar frequency. 17 switches occurred between 3 and 6 weeks of being on antipsychotic therapy. This was followed by 16 switches that occurred between 6th week and 9th week of therapy, 13 switches between 9th and 12th week of therapy, and 11 switches that occurred between initiation and 3 weeks of therapy. The most common switch was risperidone to olanzapine.
Off labelled use of antipsychotics
In our study, antipsychotics had been used off label as many as 18 (6.14%) times. Risperidone and olanzapine had been used off label 14 times constituting 4.77% of the total number of times antipsychotics had been prescribed. Clozapine (1), haloperidol (2) and fluphenazine (1) had also been used off label. The off label indications observed were organic brain syndrome, seizure disorder, obsessive compulsive disorder, organic delirium state, mental retardation and depression.
Discussion
In the present study, psychotic disorders (67.81%) were the major diagnosis amongst the 224 patients enrolled. Other diagnoses for which antipsychotics were prescribed were bipolar disorders, depressive disorders, anxiety disorders, and other off label indications. In our study, atypical and typical antipsychotics were prescribed 88.7% and 11.3% of the times an antipsychotic was prescribed, respectively. This trend is similar to the study conducted at a hospital in Rajkot[23] which reported 43.8% usage of atypical antipsychotics versus 26.3% for typical ones. In another study conducted in Calicut, atypical versus typical antipsychotics usage was 84.27% versus 15.73%, respectively which is closer to our results.[24] Similar study conducted at a Mumbai hospital found 77% usage of atypical antipsychotics. In a retrospective audit of 1591 prescriptions at a hospital in Bahrain, atypical usage was found to be 67.7%
In 224 patients enrolled in the present study, a total 293 antipsychotics were prescribed. Risperidone emerged to be the most commonly prescribed antipsychotic (44.71%) followed by olanzapine (34.81%) and aripiprazole (7.12%). A higher usage of risperidone (56.17%) had been reported in another study conducted in India.[24] The study reported olanzapine being used in 21.34% cases followed by quetiapine (3.93%). [24] Usage frequency is completely different compared to another study which reported olanzapine usage in 64% cases while risperidone was second. Similarly, of the 510 prescriptions analyzed at Kolkata, olanzapine was most commonly prescribed (77.06%).[8] The study at a Mumbai hospital had risperidone usage in 20.8% cases followed by quetiapine (19.8%).[7] A retrospective cohort analysis from a German insurance fund noted olanzapine (26.6%) and clozapine (21.3%) to be frequently prescribed.[4] Risperidone was the most frequently prescribed antipsychotic at a psychiatric hospital in Bahrain.[5] Hence, no particular antipsychotic usage seems to be uniform across different studies. However, risperidone and olanzapine seem to be most commonly prescribed overall.
In the present study, an average of 3.12 drugs were prescribed per encounter. These findings are lower than that observed (6.24) in a cross sectional study at a psychiatry outpatient department of a tertiary care hospital in Delhi.[25] It is an evidence of rational practice in our setup to have lesser number of drugs per encounter as a higher number could be a potential cause for drug interactions. However, only few (16.22%) drugs were prescribed by generic name which is very low compared to a study report at Burdwan (92.66%).[8] Other study conducted in Delhi noted 25.12% prescription by generic names.[26] The pattern of prescribing by brand names comes from increased marketing pressure by pharmaceutical companies and needs to be seriously addressed. In our country where costly drugs pose a great burden to the economically weaker section, prescribing by generic names would be a healthy practice. We did not have any patient being prescribed an antimicrobial. Overuse and misuse of antimicrobials is rampant and leads to development of resistance in the community. This observation in our study reflects judicious and restricted use of antimicrobials.[27] We also report only one instance of antipsychotic, fluphenazine injection being prescribed. This observation is in tune with the current opinion to restrict irrational use of injections.[9]
As many as 72.41% drugs were prescribed from the hospital essential medicines list. A study conducted in Delhi reported 75-95% drugs being prescribed from the essential medicines list.[26] Prescribing drugs from the essential medicines list is a vital step at encouraging rational prescription. Though majority of the drugs are prescribed from the list at our setting, there is still considerable scope of having more drugs prescribed from this list. Polypharmacy or prescribing more than four drugs may be a necessity to treat psychiatric disorders poorly controlled on monotherapy. However, such practices not only increase the probability of drug interactions and adverse drug reactions but also pose questionable effect on treatment outcome. It is a known observation that psychotropic agents acting on the central nervous system carry a high probability of causing adverse drug reactions. Extrapyramidal reactions occurring commonly due to antipsychotics are counteracted by anticholinergic agents. The addition of an anticholinergic to the prescription adds to the total number of drugs. Polypharmacy has been associated with advanced age, anticholinergic use and less use of atypical antipsychotic.[10] In the present study, total of 11 patients (4.91%) had been prescribed more than one antipsychotic on a single encounter. However, taking into consideration other concomitant medications (psychotropic agents, non-psychotropic medications and nutraceuticals), we found as many as 69.14% patients to be receiving an average of 3 drugs per encounter. Polypharmacy was found in 14.17% cases. In one study, use of more than one antipsychotic was seen in 9% cases which is more than what we found (4.91%).[24] The incidence of polypharmacy noted in other studies is quite high compared to ours. A study conducted in Singapore to evaluate polypharmacy across six south-east Asian countries evaluating records of 2399 patients reported an incidence of 45.7% with wide intercountry variations.[10] Similarly, a study conducted in Nagpur reported 61.5% prescriptions with practice of polypharmacy.[18] Similarly, incidence of 41.9% has also been reported by another Indian study.[11,12] A plausible reason for lower prevalence of antipsychotic polypharmacy in our study could be the age group of patients enrolled in the study, the exclusion of inpatients, and widespread use of atypical antipsychotics. 94.8% patients in our study were within 18-60 years while a meagre 5.2% were above 60 years. The incidence of polypharmacy has been found to be higher in the older age group. Also, we report a much higher use of atypical antipsychotics (88.7%) than any other study which could be responsible for a reduced need for polypharmacy. In the present study, antipsychotics constituted 46% of the total psychotropic agents prescribed. Sedative hypnotics, mood stabilizers and antidepressants were prescribed 34.9%, 11.16% and 7.86% of the times, respectively. The most probable reason behind prescribing other psychotropic agents could be because patients with psychiatric diagnoses besides psychotic disorders were also included in the study. All patients who were prescribed antipsychotics were included and therefore concomitant medications used recorded. Similarly, an 8.3% nutraceutical usage was also recorded. These nutraceuticals included vitamin and mineral combinations. This is in line with another study which reported use of 8.7% of the total drugs.[28] We also found anticholinergic usage to be 18.8% against antipsychotic use of 32.99% of the total drugs studied, anticholinergics being prescribed to treat extrapyramidal symptoms of antipsychotics. In a study conducted in Norway to determine co-prescription of anticholinergic and antipsychotic agents, the concurrent use of anticholinergics varied from 0.4% to 26%. The study population included 40.76% patients on atypical antipsychotic versus 59.23% on typical ones.[29] Another study conducted across 5 European countries reported a higher usage (30.1%) of anticholinergic agents among 2,725 prescriptions of patients on atypical antipsychotics.[30] A low incidence of anticholinergic use possibly implies a high usage of atypical antipsychotics which carry lower probability of causing extrapyramidal reactions. Anticholinergic co-prescription to prevent or treat extrapyramidal symptoms with antipsychotics also carries risk of adverse drug reactions like dry mouth, photophobia, constipation, etc. by virtue of blocking muscarinic receptors. Hence, the benefits of prescribing such agents needs to weighed against the risks involved. As the newly diagnosed patients on antipsychotics were enrolled in our study, we followed them up to record any switch over, augmentation or decrease in therapy. Of the 224 patients enrolled, 52 had one switch over during the course of 3 months while 3 patients had two switch overs, thus amounting to a total of 58 switches. Majority of the switches occurred with similar frequency. Of the drugs, risperidone and olanzapine were maximally switched probably due to widespread use of these drugs. The reason for switch over were lack of efficacy, adverse drug reactions, high cost or non-availability in the hospital pharmacy. We could not determine which factor contributed most to these switch overs as the number of switchovers were small enough to reach statistical significance. It was noted that maximum switches happened from week 3 till week 9 of therapy with antipsychotic agents. Any switch early in the course of therapy could be attributed to adverse drug reaction while switches later on could possibly question the efficacy of the antipsychotic. However, to ascertain whether duration of therapy has any bearing on the switch over, well designed studies need to be conducted to adjust for other variables like cost and availability. In a retrospective analysis of drug switches conducted in pediatric inpatient population at a psychiatric center in Vancuover, an effort was made to study which established pattern of switch predominates in therapy.[16] Findings in the present study are similar to their study which reported similar frequency and pattern of switches amongst the patterns of drug switches. The most common switch was risperidone to quetiapine[16] which is different from our study in which risperidone to olanzapine switch was commonest. However, the present study is first in literature, which attempts to study the type and timing of switch over in outpatients department. Off label use of psychotropic agents has been widely reported in various studies. In a study conducted in Gujarat, 39.5% drugs in psychiatry outpatients department were prescribed off label.[17] Off label use of antipsychotics was reported in 5.6% patients.[17] Likewise, a study conducted in Nagpur reported off label use of olanzapine in 28 cases.[18] In the present study, off label prescription occurred 18 (6.14%) times. Risperidone and olanzapine had been used maximally and made up 4.77% of such instances. The off label indications observed were organic brain syndrome, seizure disorder, obsessive compulsive disorder, organic delirium state, mental retardation and depression. The study was conducted focusing on existing prescription patterns, and drug utilization of antipsychotics at a tertiary care center. The use of antipsychotics for majority of the indications is in concordance with the existent guidelines and recommendation. However, off label prescribing cannot be completely negated. As is the practice worldwide, the use of atypical antipsychotics was much higher compared to older typical ones in lieu of the risk of extrapyramidal reactions associated with the latter. A rampant practice of prescribing by generic names exists, though, much of the prescribing is from the essential medicines list. Practice of prescribing more than one antipsychotic at a single visit and polypharmacy also exists in our setup, though the prevalence is low. Switching over from one antipsychotic to another appears to follow a pattern in terms of technique as well as duration of therapy. Most switches whether titrated, immediate, gap or overlapping occurred in similar frequency and mostly occurring between 3rd week and 9th week of antipsychotic therapy.
References
- Sadock BJ, Sadock VA, Sussman N. General Principles of Psychopharmacology In Kaplan and Sadock’s pocket handbook of psychiatric drug treatment, Philadelphia, Lipincott Williams and Wilkins, 2006;p.1-22.
- Padmini DD, Kumar R, Guido S. Prescription patterns of psychotropic drugs in hospitalized schizophrenic patients in a tertiary care hospital. Calicut Med J 2007;5:e3.
- Trivedi JK, Dhyani M, Yadav VS, Rai SB. Anti-psychotic drug prescription pattern for schizophrenia: Observation from a general hospital psychiatry unit. Indian J Psychiatry 2010;52:279.
- Weinbrenner S, Assion HJ, Stargardt T, Busse R, Juckel G. Drug prescription patterns in schizophrenia outpatients: analysis of data from a German health insurance fund. Pharmacopsychiatry 2009;42:66-71.
- Khalid AJAK, Mohammed KAH, Reginald PS, Adel RAO. Antipsychotic and anticholinergic drug prescribing pattern in psychiatry: extent of evidence- based practice in Bahrain. Pharmacol Pharma 2012;3:409-16.
- Grover S, Avasthi A. Anti-psychotic prescription pattern: A preliminary survey of Psychiatrists in India. Indian J Psychiatry 2010;52:257-9.
- Shrivastava A, Johnston M, Terpstra K, Stitt L, Shah N. A typical antipsychotics usage in long-term follow-up of first episode schizophrenia. Indian J Psychiatry 2012;54:248-52.
- Ghosh S, Bhattacharyya S, Dalai CK. Antipsychotic prescribing pattern in a tertiary care hospital of Eastern India. J Drug Deliv Ther 2013;3:38-42.
- De Vries TPGM, Henning RH, Hogerzeil HV, Fresle DA. Guide to Good Prescribing. A practical manual. Geneva: World Health Organisation.1994;113.
- Sim K, Su A, Fujii S, Yang S, Chong M. Antipsychotic polypharmacy in patients with schizophrenia: a multicentre comparative study in East Asia. Br J Clin Pharmacol 2004;58:178-83.
- Cuevas C, Sanz EJ. Polypharmacy in psychiatric practice in Canary Islands. BMC Psychiatry 2004;4:1-8.
- Mortimer A, Shepherd C, Rymer M, Burrows A. Primary care use of antipsychotic drugs: an audit and intervention study. Ann General Psychiatry 2005;4:1-8.
- Paton C, Lelliot P, Harrington M, Okocha C, Sensky T. Pattern of antipsychotic and anticholinergic prescribing for hospital inpatients. J Psychopharmacol 2003;17:223-29.
- Chong M, Tan C, Fujii S, Yang S, Ungvari G. Psychiary and clinical Neurosciences 2004;58:6167.
- Freudenreich O, Goff DC. Antipsychotic combination therapy in schizophrenia. A review of efficacy and risks of current combinations. Acta Psychiatr Scand 2002;106:323-30.
- Linton A. A retrospective study of antipsychotic drug switching in a pediatric population. BMC Psychiatry 2013;13:248.
- Kharadi D, Patel K, Rana D, Patel V. Off-label drug use in Psychiatry Outpatient Department: A prospective study at a Tertiary Care Teaching Hospital. J Basic Clin Pharma 2015;6:45-9.
- Deshmukh SA, Ismail TS. Evaluation of psychotropic drugs use pattern among out patients attending psychiatry department at Government Medical College and Hospital, Nagpur: A cross sectional study. Int J Pharm Bio Sci 2012;3:428-36.
- How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators - EDM Research Series No. 007.
- Remington G, Chue P, Stip E, Kopala L, Girard T. The crossover approach to switching antipsychotics: what is the evidence? Schizophr Res 2005;76:267–72.
- Buckley PF, Correll CU. Strategies for dosing and switching antipsychotics for optimal clinical management. J Clin Psychiatry 2008;69:4–17.
- Lambert TJ. Switching antipsychotic therapy: what to expect and clinical strategies for improving therapeutic outcomes. J Clin Psychiatry 2007;68:10–13.
- Piparva K, Singh A, Trivedi H, Parmar D, Gajera M. Drug utilization study of psychotropic drugs in outdoor patients in a teaching hospital. Indian J Psychol Med 2011;33:54.
- Padmini DD, Kumar R, Guido S. Prescription patterns of psychotropic drugs in hospitalized schizophrenic patients in a tertiary care hospital. Calicut Med J 2007;5:e3.
- Jhanjee A, Bhatia MS, Oberoi A, Srivastava S. Medication errors in psychiatric practice- A cross sectional study. Delhi Psychiatry J 2012;15:5-13.
- Biswas NR, Biswas RS, Pal PS, Jain SK, Malhotra SP. Patterns of prescriptions and drug use in two tertiary hospitals in Delhi. Indian J Physiol Pharmacol 2000;44:109-12.
- Antimicrobial resistance. World Health Organization. 2012.
- Roopadevi HS, Ramesh KN, Nagabushan H. Pattern of psychotropic prescription in a tertiary care teaching hospital: a critical analysis. Asian J Pharm Clin Res 2015;8:252-5.
- Gjerden P, Slørdal L, Bramness J. Association between the use of anticholinergic antiparkinson drugs and safety and receptor drug-binding profiles of antipsychotic agents. Eur J Clin Pharmacol 2009;65:1229-35.
- Broekema W, Groot I, Harten P. Simultaneous prescribing of atypical antipsychotics, conventional antipsychotics and anticholinergics-a European study. Pharm World Sci 2007;29:126-30.