An evaluation of the prescribing patterns for under-five patients at a Tertiary Paediatric Hospital in Sierra Leone
- *Corresponding Author:
- Dr. Christine Princess Cole
Department of Clinical Pharmacy and Therapeutics, Faculty of Pharmaceutical Sciences, College of Medicine and Allied Health Sciences, University of Sierra Leone, Sierra Leone.
E-mail: cpcole2003@yahoo.co.uk
Abstract
Purpose: There is limited information on pediatric prescribing in Sierra Leone. This study evaluated prescribing patterns for under‑five patients at Ola During Children’s Hospital (ODCH) and assessed the extent of rational prescribing. Methods: A descriptive, cross‑sectional, retrospective study of 294 prescriptions, selected by systematic random sampling was conducted at the outpatient department of ODCH. The World Health Organisation prescribing indicators were analyzed using the SPSS package 16.0. The index of rational drug prescribing (IRDP) was calculated to assess rational prescribing. Results: The average number of medicines per prescription was 3.77. The percentage of medicines prescribed by generic names was 71.0%, while 74.8% and 21.1% of prescriptions had an antibiotic and injection, respectively. The percentage of medicines prescribed from the national essential medicines list was 70.6%. The most commonly prescribed pharmacological groups of medicines were vitamins (85.37%) and antibiotics (82.99%). The IRDP was 2.71, instead of the ideal value of 5. Conclusion: Pediatric prescribing patterns at the outpatient department of ODCH cannot be said to be entirely rational, especially with regards to antibiotic and injection prescribing.
Keywords
Antibiotics, essential medicines list, generics, injections, rational prescribing, under‑five
Introduction
The use of medicines is known to be one of the most effective therapeutic interventions in health care today, especially when utilized responsibly. The World Health Organisation (WHO) defines rational medicines use as when a “patient receives medications appropriate to clinical needs, in doses that meet their individual requirements, for an adequate period of time and at the lowest cost to them and their family.”[1] This is known to have medical, social and economic benefits both to the individual and the society.[2] On the other hand, irresponsible use of medicines has been identified as a major problem in healthcare worldwide; for instance, WHO estimates that at least 50% of all medicines are used irrationally.[3] In developing countries where 20–50% of health budgets are spent on drugs and other health commodities,[4] irrational medicines use has been documented to contribute to patient morbidity and mortality, increase individual and government spending, as well as reducing confidence in the health care system.[5] It can take the form of self‑medication, misuse and underuse of drugs, polypharmacy, unnecessary use of antibiotics and injections, as well as inappropriate prescribing discordant with clinical guidelines.[3]
Sierra Leone is a developing country with a projected population of 6.2 million people in 2014.[6] Children below 5 years constitute 17.7% of the total population.[7] They are known to be vulnerable to contracting disease and to the harmful effects of medicines. Drug prescribing in this cohort is known to be especially challenging due to peculiarities in organ function and disease state reflecting their age, the paucity of pharmacokinetic, pharmacodynamic, safety and efficacy data for these patients, ethical, financial and regulatory limitations and lack of provider training in pediatric pharmacotherapy.[8,9] Therefore, irrational use of medicines including prescribing in this group of patients has been documented to be widespread.[10] For instance, an increased prevalence of adverse drug reactions, self‑medication by carers and excessive use of antibiotics have been documented among pediatric patients in the African region.[11‑13] Irrational medicine use among this population is further hampered by off‑label use of medicines, counterfeit and substandard products, drug shortages, and unregulated advertising.[14] Also, irrational prescribing has been identified as a risk factor for developing adverse drug reactions and medication errors in infants.[15] Furthermore, determinants of irrational prescribing by doctors include patient demands or expectations, lack of appropriate role models to copy from, lack of objective drug information, and vigorous drug promotion by drug companies.[16‑18] Thus, it is vital to study the drug use pattern of doctors in this population with the aim to optimizing drug therapy.
The introduction of the free health care initiative in Sierra Leone 4 years ago for under‑fives, pregnant women, and lactating mothers has seen an increased utilization of health services including drugs.[19,20] However, its impact on an infant (92 death/1000 births) and under‑five (156 deaths/1000 births) mortality rates still remain minimal.[21] Although, the causes of these high indices are attributed to preventable diseases such as diarrhea, pneumonia, and malaria, irrational medicines use, especially inappropriate prescribing, could also be a contributing factor.
In order to describe the drug use situation in health facilities, WHO developed a set of standardized drug use indicators which can provide a basis for planning and implementation of rational medicine use strategies if any problems are identified. Specifically, the prescribing indicators are useful in identifying problems in general prescribing. They include the following: Average number of drugs per encounter (measuring the degree of polypharmacy), percentage of drugs prescribed by generic name (which measures the cost‑effectiveness of a health system to procure and use drugs), the percentage of encounters with an antibiotic and injection prescribed (measures the level of use of two important, but commonly overused and costly forms of drug therapy) and the percentage of drugs prescribed from the national essential medicines list (NEML).[22]
Studies in the African region and India have been carried out using these WHO indicators in many health facilities among pediatric populations. For instance, the studies on drug prescribing at a children’s outpatient clinic and at a Teaching Hospital in Nigeria, [23,24] prescribing in pediatric wards in Ethiopia [25] and prescribing practices in the pediatric department of a North Indian University Hospital,[26] to name a few. These studies have indicated the irresponsible use of medicines in the form of polypharmacy, increased prescription of antibiotics and injectables and non‑adherence to national treatment guidelines and or essential medicines lists (EML). In Sierra Leone, no such study has been done so far regarding rational drug use in pediatric patients, especially under‑fives. To address this gap, we decided to evaluate the prescribing patterns for under‑five patients at a tertiary pediatric hospital in Sierra Leone using the WHO recommended prescribing indicators for drug use and further assess rational prescribing performance using the Index of Rational Drug Prescribing (IRDP).
Methods
Study setting
This study was conducted at the Ola During Children’s Hospital (ODCH), the Only Tertiary Paediatric Hospital in the Sierra Leone located at the east end of the capital city Freetown. It is the referral center for pediatric cases from primary and secondary health facilities countrywide. It also serves as one of the teaching hospitals of the College of Medicine and Allied Health Sciences, University of Sierra Leone (COMAHS‑USL).
Study design and population
A descriptive, cross‑sectional, retrospective study, which examined prescriptions from October to December, 2013 was conducted. The study population included all patients under‑five years of age who were seen by doctors at the outpatient department of ODCH and for whom medicines were prescribed. The sampling frame included the prescriptions of all under‑five patients seen by doctors at the outpatient department of the ODCH. Prescriptions for the 3 months under review were arranged by dates and those used for the study were selected using systematic random sampling. A total of 294 prescriptions were sampled.
Data collection
A data collection tool was used to collect information on patient demographics (age and sex), prescribing indicators and pharmacological classes of drugs prescribed from prescription records at the hospital pharmacy of ODCH. Prescriptions outside the study period, those for inpatients and patients above 5 years of age were excluded.
Ethical approval
Ethical clearance was obtained from the COMAHS Research and Ethics Committee and informed consent was obtained from the hospital administration.
Data analysis
The patient demographic data, WHO prescribing indicators (average number of medicines prescribed per patient encounter, percentage of drugs prescribed by generic name, percentage of encounters with an antibiotic prescribed, percentage of encounters with an injection prescribed and percentage of medicines prescribed from the NEML) and pharmacological classes of medicines prescribed were analyzed using the Statistical Package for Social Sciences (SPSS) version 16.0. SPSS, Inc; Chicago, USA. Descriptive statistics was used to calculate frequency counts, averages, and percentages.
The IRDP was determined by adopting a previously validated method [27] used by Dong et al.[28] It consists of five indices derived from the WHO prescribing indicators mentioned above. The optimal level for each indicator is shown Table 1.[29,30] Each of the five prescribing indicators has an optimal index of 1; the closer to 1 the calculated index is, the more rational prescribing is considered to be. The index of polypharmacy was measured by the percentage of nonpolypharmacy prescriptions; in this study, those prescriptions with three or less medicines where considered as nonpolypharmacy. The generic name index and essential medicine index were measured by the percentage of drugs prescribed by generic name and from the NEML respectively. The index of rational antibiotic prescribing was defined as dividing the optimal level (30%) by the percentage of prescriptions including antibiotic. The index of safety injection was calculated by dividing the optimal level (10%) by the percentage of prescriptions including the injection. The IRDP, which has a maximum value of 5, can then be calculated by adding the indices.
| Prescribing indicators | Optimal level (%) | Optimal index |
|---|---|---|
| Percentage of nonpolypharmacy prescriptions | ≤3 | 1 |
| Percentage of drugs prescribed by generics | 100 | 1 |
| Percentage of prescriptions including antibiotics | ≤30 | 1 |
| Percentage of prescriptions including injections | ≤10 | 1 |
| Percentage of drugs prescribed from EML or formulary | 100 | 1 |
EML: Essential medicines list
Table 1: Optimal levels of drug prescribing indicators.
Results
Demographic data of patients
The majority of the patients were between the age bracket of 29 days to 24 months and over half of them were male [Table 2].
| Number (%) | ||
|---|---|---|
| Age | ||
| 0-28 days | 7 | (2.4) |
| 29 days to 12 months | 82 | (27.9) |
| 13-24 months | 85 | (28.9) |
| 25-36 months | 40 | (13.6) |
| 37-48 months | 26 | (8.8) |
| 49-60 months | 54 | (18.4) |
| Sex | ||
| Male | 172 | (58.5) |
| Female | 122 | (41.5) |
ODCH: Ola During Children’s Hospital
Table 2: Demographic data of under-five patients seen at the outpatient department of ODCH (original).
Prescribing indicators
The average number of medicines per prescription was 3.77 ranging from 1 to 8. Seventy‑one percent (71.0%) of these were prescribed as generics and 70.6% prescribed from the NEML [Table 3]. Seventy‑five percent (74.8%) and 21.1% of the prescriptions had at least an antibiotic and an injection prescribed respectively [Table 3].
| Prescribing indicator | Average/percentage |
|---|---|
| Average number of medicines prescribed per encounter | 3.77 |
| Percentage of drugs prescribed by generic name | 71.0 |
| Percentage of encounters with an antibiotic prescribed | 74.8 |
| Percentage of encounters with an injection prescribed | 21.1 |
| Percentage of medicines prescribed from the NEML | 70.6 |
ODCH: Ola During Children’s Hospital, NEML: National essential medicines list
Table 3: Prescribing indicators at the outpatient department of ODCH (original).
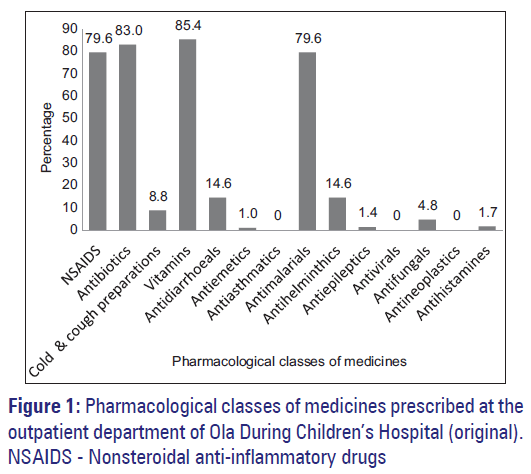
Pharmacological class of medicines prescribed
The most common prescribed medicines were the vitamins (85.4%), antibiotics (83.0%), nonsteroidal anti‑inflammatory drugs (NSAIDS) (79.6%) and antimalarials (79.6%). Figure 1 shows the different classes of medicines prescribed by doctors at the outpatient department of ODCH.
The index of rational drug prescribing
The IRDP used as an indicator of rational drug use was 2.71. Antibiotic prescribing, polypharmacy and injection prescribing had the lowest indices of 0.40, 0.42 and 0.47, respectively. Table 4 depicts the IRDP of doctors who worked at the outpatient department of ODCH.
| Index of | Generic | Index of rational | Index of rational | Essential | IRDP |
|---|---|---|---|---|---|
| polypharmacy | prescribing index | antibiotic prescribing | injection prescribing | medicines index | |
| 0.42 | 0.71 | 0.40 | 0.47 | 0.71 | 2.71 |
IRDP: Index of Rational Drug Prescribing
Table 4: IRDP (original).
Discussion
The results of this study provide valuable information on the prescribing patterns of doctors for under‑five patients at a Tertiary Paediatric Hospital in Sierra Leone. Many of the patients seen were 29 days to 24‑month‑old and there were more males than females, similar to that obtained in a study of pediatric outpatients at a Tertiary Teaching Hospital in Lagos, Nigeria.[23]
Polypharmacy is prescribing more medicines than are clinically indicated or the use of an excessive number of inappropriate medicines. An average of four medicines was prescribed per patient encounter in this study, indicating the presence of polypharmacy as this is higher than the optimal value of <3 drugs. This is comparable to the results of similar studies done among pediatric patients in Nigeria,[23,24] Ethiopia [31] and in India [32] but in contrast to another in the Gambia in which fewer medicines were prescribed.[33] Pressure on prescribers from caregivers to prescribe medication for every symptom or condition‑even minor ones and the robust drug promotion by pharmaceutical companies are known to influence doctor’s prescribing practices. These factors might have contributed to the polypharmacy observed in this study. Polypharmacy is known to increase health care cost; prolong hospital stay due adverse reactions and drug interactions. Therefore, the overprescribing of medicines observed in this study has the tendency to undermine one of the major objectives of the Free Health Care Initiative in Sierra Leone which is the reduction of the currently high infant and under‑five mortality rates. Although not considered in this study, the impact of the irrational use of medicines in general on the currently run free healthcare initiative for under‑five children in Sierra Leone is an area that needs further research.
Generic prescribing has been found to reduce the cost of medicines and also promote better communication among healthcare providers [34] which is of great importance in developing countries like Sierra Leone. In the past decade, an increased trend in generic prescribing in developing and transitional countries has been observed [35] and this resonates with our results in which 71% of all the medicines prescribed during the study period were generics. This is also in line with the results of a similar study done in the Gambia [33] but different from those conducted in Nigeria [23,24] and in India [32] in which <41% of medicines prescribed were generics. The high generic prescribing index seen in this study is likely due to increased compliance by prescribers to using the NEML as seen by the high percentage (71%) of drugs that were prescribed from it. The increased monitoring mechanism by the free health care initiative ensuring that medicines are prescribed from the EML, of which most are generics, might have had a huge impact. Essential medicines are those that satisfy the priority health care needs of the population, selected with due regard to public health relevance, evidence on efficacy and safety, and comparative cost‑effectiveness.[36] Prescribing from an essential medicine list has also increased progressively over the past 25 years globally [35] and results from studies in the African region [23,24,37] have also recorded a similar pattern. The implementation of the WHO essential medicine program in many African countries over the past decade has contributed to the increased compliance observed.
An increase in the inappropriate use of antibiotics has been reported globally, driven by financial and budgetary constraints, market forces, distortion and behavior of health systems, health practitioners, and drug companies. The development of resistance as a result of irresponsible antibiotic use is known to cause prolonged hospital stay, suboptimal therapeutic outcomes leading to death and increased healthcare expenditure.[38] In our study, antibiotics were prescribed in about three‑quarters of patient encounters at ODCH. This high rate of prescribing antibiotics appears to be a common trend in developing countries as evident from findings in the Gambia, [33] Ethiopia [39] and in India.[32] In such countries, children are at risk of losing their lives to otherwise treatable infections due to the development of resistance to lifesaving antibiotics. The irrational use of antibiotics evident from the low antibiotic prescribing index observed in this study might be a contributing factor to the disturbingly high infant and under‑five mortality in Sierra Leone. Nonadherence to standard treatment guidelines has been reported among pediatric patients in rural Sierra Leone.[40] This might also be the case at ODCH and can be considered a contributing factor to the irrational prescribing of antibiotics observed in this study. Programs targeted at health providers designed to promote the rational use of medicines, especially antibiotics are highly needed if the overall aim of the free healthcare initiative is to be achieved.
The increased utilization of injections as a form of irrational medicines use is also a public health concern. It has been documented to contribute to increase hospital waste where waste management systems are not fully efficient, incurs unnecessary pain to the patient, promote the spread of infections like HIV/AIDS, hepatitis and abscesses and promote microbial resistance, muscle contractures and nerve injury. Furthermore, irrational prescribing of antibiotics and injections is expensive in terms of health care cost and health staff time adding extra strain on the already weak health infrastructure.[3] In this study, injections were being prescribed more than necessary, with at least 20% (IRDP of 0.47) of all prescriptions at ODCH having at least one injection. This is similar to that reported by Oshikoya et al. in Lagos, Nigeria.[23] Comparatively, much lower injection prescribing rates were noted in other studies among under‑fives in Owerri, Nigeria [24] and among pediatric patients in India.[32] Anecdotal evidence suggests that most parents or guardians prefer injections for their children as they consider it more effective in treating disease than other dosage forms. The increased use of injections in this study might be explained by doctors being under pressure to prescribe them from caregivers.
Finally, our study also revealed that vitamins, antibiotics, NSAIDS and antimalarials were the most commonly prescribed pharmacological group of medicines for this group of patients at ODCH. This result is also in line with others done in Nigeria [23] and Ethiopia [31,41] in which antimicrobials, preferably penicillins were the most common medications use. These commonly prescribed medications are a reflection of the pattern of disease burden in the country, as malaria (41%), respiratory tract infections (17%), anemia (12%) and diarrhea (5%) are the major causes of hospital deaths among under‑fives in Sierra Leone.[42] NSAIDS and to a lesser extent antibiotics predispose to upper gastrointestinal complications in children, [43] which further re‑echoes the need for their rational use. Further studies are thus needed to determine the appropriateness of prescribing these medicines and to provide more conclusive evidence as to whether they are prescribed rationally or not.
The strength of this study is that it provides baseline information on rational pediatric prescribing to which future assessments can be compared when monitoring prescribing trends and providing interventions if needed. However, certain limitations exist. For instance, this is a purely descriptive study, and the appropriateness of and underlying reasons or factors influencing prescribing, especially with regards to antibiotics and injections were not assessed. Furthermore, how appropriately medications were prescribed with regards to a specific disease was also not considered in this study. Furthermore, prescribing patterns for inpatients was also not evaluated. This makes it difficult to develop and implement appropriate intervention (s) that promote rational prescribing. Further studies will, therefore, be needed to address these limitations.
Conclusion
Prescribing for under-five out patients at ODCH is far from being rational and needs improvement, especially with respect to polypharmacy, antibiotic and injection prescribing, as is evident from the low IRDP (2.71 out of 5) reported. This impedes efforts to reduce infant and under-five mortality and minimize undue health care costs and is of concern because as a Tertiary Referral Paediatric Hospital in Sierra Leone, patient care should be of the highest quality. The provision of continuous in-service prescribing education for prescribers and regular evaluation of prescriptions are needed./p>
Source of Support: Nil
Conflict of Interest: None declared.
References
- WHO. The Rational Use of Drugs. Report of a Conference of Experts, Nairobi, 25-29 November 1985. Geneva: WHO; 1987.
- Teferra A, Zeruesenay D, Asfawossen GY. Prescribing pattern of drugs in medical wards of three hospitals in northwest Ethiopia. J Ethiop Med Pract 2002;4:8-13.
- WHO. Promoting rational use of medicines: Core components. WHO Policy Perspectives on Medicines. Geneva: WHO; 2002. p. 1-6.
- World Bank. The importance of pharmaceutical and essential drug programs: Better Health in Africa, Experience and Lessons Learned. Washington, D C: World Bank; 1994.
- Thawani V. Rational use of medicines: Achievements and challenges. Indian J Pharmacol 2010;42:63-4.
- Koroma DS, Turay AB, Moigua MB. Republic of Sierra Leone: 2004 Population and Housing Census: Analytical Report on Population Projection for Sierra Leone. Freetown: Statistics Sierra Leone; 2006.
- Statistics Sierra Leone; Ministry of Health and Sanitation Sierra Leone; ICF International USA. Sierra Leone Demographic and Health Survey, 2008. Calverton, Maryland, USA: Statistics Sierra Leone; 2009.
- Clavenna A, Berti A, Gualandi L, Rossi E, De Rosa M, Bonati M. Drug utilisation profile in the Italian paediatric population. Eur J Pediatr 2009;168:173-80.
- Oshikoya KA, Senbanjo IO. Providing safe medicines for children in Nigeria: The impediments and remedies. Ann Afr Med 2010;9:203-12.
- Hogerzeil HV. Promoting rational prescribing: An international perspective. Br J Clin Pharmacol 1995;39:1-6.
- Oshikoya KN, Njokanma OF, Chukwura HA, Ojo IO. Adverse drug reactions in Nigerian children. Paediatr Perinat Drug Ther 2007;8:81-8.
- Oshikoya KA, Senbanjo IO, Njokanma OF. Self-medication for infants with colic in Lagos, Nigeria. BMC Pediatr 2009;9:9.
- Eldalo AS, Moula NM, Yousif M. Antibiotics prescribing pattern in hospitalized paediatric patients, Khartoum state, Sudan. Ribat J Med Sci 2012;1:38-44.
- WHO. Promoting Safety Of Medicine for Children. Geneva: WHO; 2007.
- Oshikoya KA, Ojo OI. Medication errors in paediatric outpatient prescriptions of a teaching hospital in Nigeria. Nig Q J Hosp Med 2007;17:74-8.
- Stanulovic M, Jakovljevic V, Roncevic N. Drug utilization in paediatrics: Non-medical factors affecting decision making by prescribers. Eur J Clin Pharmacol 1984;27:237-41.
- Bhatt AD. Drug promotion and doctor: A relationship under change J Postgrad Med 1993;39:120-3.
- Chaturvedi VP, Mathur AG, Anand AC. Rational drug use – As common as common sense Med J Armed Forces India 2012;68:206-8.
- Diaz T, George AS, Rao SR, Bangura PS, Baimba JB, McMahon SA, et al. Healthcare seeking for diarrhoea, malaria and pneumonia among children in four poor rural districts in Sierra Leone in the context of free health care: Results of a cross-sectional survey. BMC Public Health 2013;13:157.
- Maxmen A. Sierra Leone’s free health-care initiative: Work in progress. Lancet 2013;381:191-2.
- Statistics Sierra Leone; Ministry of Health and Sanitation Sierra Leone; ICF International USA. Sierra Leone Demographic Health Survey Survey 2013. Freetown, Sierra Leone, Rockville, Maryland: Statistics Sierra Leone, ICF International USA; 2014.
- WHO. How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators. Geneva: WHO; 1993.
- Oshikoya KA, Chukwura HA, Ojo OI. Evaluation of outpatient paediatric drug prescriptions in a teaching hospital in Nigeria for rational prescribing. Paediatr Perinat Drug Ther 2006;7:183-8.
- Nwolisa CE, Erinaugha EU, Ofoleta SI. Prescribing practices of doctors attending to under fives in a children’s outpatient clinic in Owerri, Nigeria. J Trop Pediatr 2006;52:197-200.
- Abula T, Desta Z. Prescribing pattern of drugs in pediatric wards of three Ethiopian hospitals. Ethiop J Health Dev 1999;13:135-40.
- Akhtar MS, Divya V, Pillai K, Kiran D, Roy MS, Najmi AK, et al. Drug prescribing practices in paediatric department of a North Indian university teaching hospital. Asian J Pharm Clin Res 2012;5:146-9.
- Zhang Y, Zhi M. Index system, appraising method for comprehensive appraisal. J North Jiaotong Univ 1995;19:393-400.
- Dong L, Yan H, Wang D. Drug prescribing indicators in village health clinics across 10 provinces of Western China. Fam Pract 2011;28:63-7.
- De Joncheere K. Implementation of Rational Pharmacotherapy. Meeting under Danish EU presidency. Perspectives and achievements with Rational Pharmacotherapy. Copenhagen Denmark, WHO/EURO; 2002.
- Melander A. Variation in drug utilization in the EU: Causes and consequences as illustrated by antibiotics. Meeting under Danish EU presidency. Perspectives and Achievements with Rational Pharmacotherapy. Copenhagen, Denmark: WHO/EURO; 2002.
- Teni FS, Surur AS, Getie A, Alemseged A, Meselu M. Medication prescribing pattern at a pediatric ward of an Ethiopian hospital. Int J Pediatr 2014;2:23-30.
- Pandey AA, Thakre SB, Bhatkule PR. Prescription analysis of pediatric outpatient practice in nagpur city. Indian J Community Med 2010;35:70-3.
- Risk R, Naismith H, Burnett A, Moore SE, Cham M, Unger S. Rational prescribing in paediatrics in a resource-limited setting. Arch Dis Child 2013;98:503-9.