A study of the prevalence of thalassemia and its correlation with liver function test in different age and sex group in the Chittagong district of Bangladesh
- *Corresponding Author:
- Robiul Hasan Bhuiyan
Department of Biochemistry & Molecular Biology University of Chittagong, Chittagong-4331, Bangladesh
E-mail: talhabmb@gmail.com
Abstract
Thalassemia is the name of a group of genetic, inherited disorders of the blood. More speciô€ÂÂÂÂically, it is a disorder of the hemoglobin molecule inside the red blood cells. According to World health Organization (WHO), there are about 3% beta-thalassemia carrier and about 4% Hb E/beta-thalassemia carrier in Bangladesh. Our objective is to identify the prevalence of beta-thalassemia in our adolescent populations and to review risk factors that would most easily identify a subset of adolescent patients at greatest risk for the development of beta-thalassemia. We also made a study of clinical proô€ÂÂÂÂile of 53 thalassemic patients, observing the relationship between the patients with their verity ages and sex. The cases are taken on the basis of their age (2-30 years), beta-thalassemia major, clinical jaundice with history of chronic blood transfusion. The cases excluded those who had jaundice due to viral hepatitis or hepatitis due to heavy metal poisoning (Arsenic) and those with spleenectomy. Liver function test has been evaluated in 53 patients. That were recorded with some relevant demographical data such as age, sex, blood group where median age was of 16 years and mean (±SD) age 15.4151 ± 7.90918. Among them were 21 (39.6%) female and 32 (60.4%) male. With an average 15.1% (8 in no.) beta-thalassemia, 7.5% (4 in no.) beta-thalassemia major and 77.4% (41 in no.) E-beta-thalassemia cases have been found in the study. Mean (±SD) TSB in total 53 subjects with age group 2-10 years and 21-30 years is signiô€ÂÂÂÂicant. The study revealed that in thalassemic patients when the age is more, the disease progresses with their complication. Hepatic complication is mainly due to being hepatocellular in nature than that of obstructive one.
Keywords
Beta-thalassemia, Chittagong, liver function test, spleenectomy, total serum billirubin, world health organization
Introduction
Thalassemia is the most common genetic blood disease in the world and varies in different population group in the world. [1] World Health Organization (WHO) estimates that at least 6.5% of the world populations are carries of different inherited disorders of hemoglobin. [2] Another WHO report estimates that 3% are carriers of beta-thalassemia and 4% are carriers of Hb E in Bangladesh. In Bangladesh, more than 7000 children are born with thalassemia each year. [3] Majority are born in countries with limited resources where priority tends to be given to tackling high rates of infant and child mortality from infection diseases and malnutrition. [4] The patients suffering from beta-thalassemia major and Hb E/ beta-thalassemia do not survive for more than 5 years without blood transfusion. [5] Thalassemia (also known as Mediterranean anemia, Cooley’s anemia, Beta-thalassemia or Alpha-thalassemia) is an inherited blood disorder affected by an abnormal form of hemoglobin blood disorder is the most common inherited single gene disorder in the world [Figure 1]. This specific type of blood disease results in excessive destruction of red blood cells which in turn leads to anemia. [6] For a better understanding of this disease one must know the importance of hemoglobin. [7] In vertebrates, hemoglobin is the iron-containing oxygen-transport protein that is found in red blood cells which carries oxygen from the lungs to the rest of the body and then brings the carbon dioxide back to the lungs to be dispensed. People who have thalassemia produce fewer healthy hemoglobin proteins, and their bone marrow produces fewer healthy red blood cells. With too few normal red blood cells, not enough hemoglobin is available to help carry oxygen to the body. [8] Thalassemia occurs more often among certain ethnicities, including people of Italian, Greek, Middle-eastern, Asian and African descent. Thalassemia is an inherited disorder which means they are passed from parents to their children. [8] a- thalassemia occurs commonly in the people of those from Southeast Asia, the Middle-east, China and those of African-American descent. [9] b- thalassemia occurs commonly in people of the Mediterranean region, Chinese, other Asians and African-Americans. [10]
In Bangladesh, a study carried out by the Dhaka Shishu Hospital Thalassemia Center in 2004 in school children of Bangladesh, showed that carrier status is higher and there is also regional variation. This study revealed that the overall prevalence of beta-thalassemia trait in Bangladesh was 4.1% and Hb E trait 6.3%. [11] A recent study showed that carrier status of Hb-E is 6.1% and as high as 40% in tribal children in Bangladesh. [12]
Materials and Methods
The study was designed on the basis of prospective observational type of study. In the study the current data was obtaining form a specific diseased group with a progressive complication. The total procedure of the study was conducted in the Thalassemia Sheba Kendro, Jamalkhan, Chittagong and also in the Biochemistry Lab, Chattagram Maa-O-Shishu General Hospital (CMOSGH), Agrabad, Chittagong.
Subject collection and study procedure
Subjects were collected on every working day of the week from 10:00 am to 2:00 pm from the Thalassaemia Sheba Kendro and when needed from the Biochemistry Laboratory in the CMOSGH. This prospective study involved patients who admitted into the Sheba Kendro for the purpose of blood transfusion and for getting iron chelation therapy. Parents or guardians were informed of the purpose of the study. For each patient a detailed history was taken from mother or the attendant. After taking brief history preliminary selection was done, and the purpose to the study was explained in details to its subject. After taking consent from the parents, data was collected, which included sex, age at presentation, age at diagnosis and clinical symptoms at presentation. A thorough physical examination was done in each patient. Majority of the patients diagnoses were confirmed by Hb-electrophoresis. The patients who fulfilled the inclusion criteria were included for this study. All the planned information obtained and recorded in the data collecting sheet properly. A total of 53 subjects were included in this study. There was no specific preference for race, religion and socioeconomic status.
Inclusion Criteria: Patients with confirmed diagnosis of thalassemia were randomly selected as first as diagnosis up to the age 30. [13] The subjects on regular blood transfusions were enrolled. The inclusion criteria considered in data collection are: (1) Thalassemia major, (2) History of jaundice other than viral, alcohol or heavy metal induces jaundice, (3) Repeated blood transfusion, (4) History of taking iron chelating therapy and (5) Clinically diagnosed Hepatomegaly.
Exclusion Criteria: There is more problem to exclude subject only basis on clinical questionnaire and on the basis of some laboratory test. [14] The exclusion criteria are as follows: (1) Thalassemia trait or intermedia type, (2) History of jaundice due to viral, alcoholic or heavy metal induces, (3) History of spleenectomy, (4) Age more than 30 years.
Additional investigations done were:
• Observation of liver function test (LFT; Serum billirubin) in different thalassemic patients.
• Estimation of serum billirubin (Jendrassik and Grof method) by spectrophotometric/ filter photometric test.
Estimation of serum billirubin by spectrophotometric/ filter photometric test
Conjugated (direct) billirubin in serum is coupled with diazotized sulfanillic acid to form red-colored compound. Ascorbic acid is used to stop the coupling reaction and to eliminate interference by hemoglobin. Caffeine benzoate solution is used to split the unconjugated billirubin protein complex releasing the billirubin so that it can react with diazotised sulfanillic acid.
The tartrate buffer makes the mixture alkaline and converts the red acid billirubin to a green-colored compound which shows peak absorbance at 607 nm. At this wavelength the absorbance due to hemoglobin or carotene is minimal. [15]
Statistical analysis
Statistical analysis was carried out using SPSS statistical package (version 11.5). Analysis of variance (ANOVA) of the data was used to detect overall difference in group means. Differences among group means were assessed using least significance difference (LSD).
Observation and results
Clinico-hematological study of thalassemia was done on 53 patients during the period of September 2011 to June 2012. Salient features observed in this study were:
Age
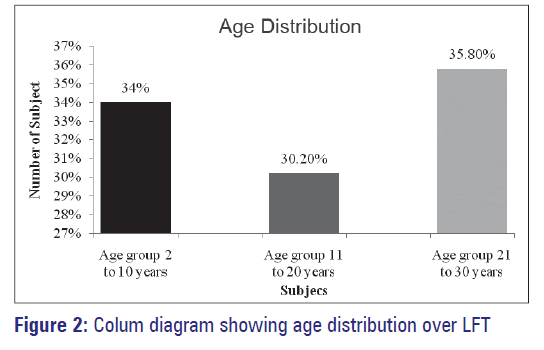
Mean (±SD) age in total 53 patients between the age group 2 and 10 years was 6.444 ± 2.61719, between 11 and 20 years mean was 15.1875 ± 3.10309 and between age 21 and 30 years mean was 24.1053 ± 2.44710 were include in the study [Table 1 and Figure 2].
| Subjects | No. of subject (%) |
|---|---|
| Age group 2-10 years | 34 |
| Age group 11-20 years | 30.2 |
| Age group 21-30 years | 35.8 |
Table 1: Group statistics of LFT with age distribution
Sex
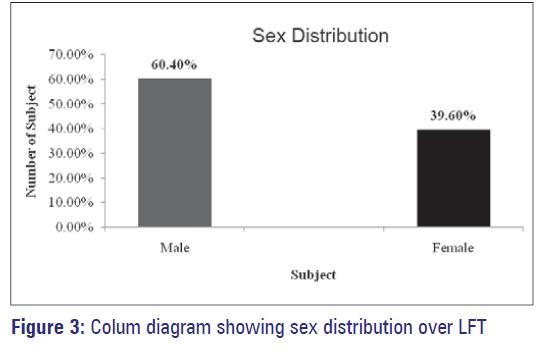
Mean (±SD) of sex in 53 no. of patients in male sex 15.000 ± 7.95147 and females are 15.9524 ± 8.00922 [Table 2 and Figure 3].
| Subject | No. of subject (%) |
|---|---|
| Male | 60.4 |
| Female | 39.6 |
Table 2: Group statistics of LFT with sex distribution
Type of thalassaemia
Frequency of the type of thalassemia E-beta-thalassemia 41 in no. (77.4%), beta-thalassemia 8 in no. (15.1%) and beta major 4 in no. (7.5%).
Total serum billirubin (TSB, mg/dl)
Mean (±SD) TSB in total 53 patients with age 2-10 years and 11-20 years are 4.7056 ± 1.91694 and 5.8188 ± 2.24773, respectively [Table 3]. Statistically no significant billirubin difference was observed between these two groups. P > 0.363
| Subjects | No. of subjects |
|---|---|
| Age 2-10 years | 4.7056 ± 1.91694 |
| Age 11-20 years | 5.8188 ± 2.24773 |
| F/p | –1.111319/0.363 |
P is not significant
Table 3: Group statistics for TSB (mg/dl) levels between age 2 and 10 and age 11 and 20 years
Mean (±SD) TSB in total 53 patients with age group 11-20 years and age 21-30 years are 5.8188 ± 2.24773 and 7.3737 ± 2.01020, respectively [Table 4]. Statistically no significant billirubin difference was observed between these two groups. P > 0.091
| Subjects | No. of subjects |
|---|---|
| Age 11-20 years | 5.8188 ± 2.24773 |
| Age 21-30 years | 7.3737 ± 2.01021 |
| F/p | –1.55493/0.91 |
P is not significant
Table 4: Group statistics for TSB (mg/dl) levels between age 11 and 20 and age 21 and 30 years
Mean (±SD) TSB in total 53 patients with age group 21-30 years and 2-10 years are 7.3737 ± 2.01021 and 4.7056 ± 1.91694, respectively [Table 5]. Statistically significant billirubin difference was observed between these two groups. P < 0.001
| Subjects | No. of subjects |
|---|---|
| Age 2-10 years | 4.7056 ± 1.91694 |
| Age 21-30 years | 7.3737 ± 2.01021 |
| F/p | 2.66813/0.001 |
P is not significant
Table 5: Group statistics for TSB (mg/dl) levels between age 2 and 10 and age 21 and 30 years
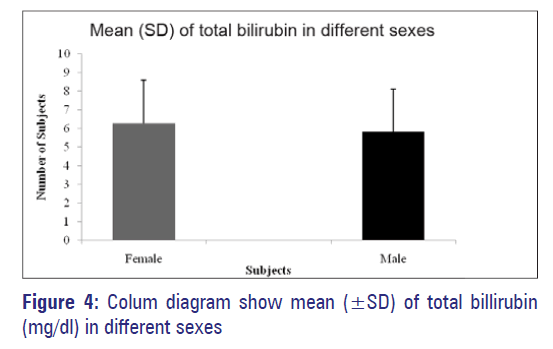
Mean (±SD) TSB in total 53 patients with different sex group are 6.2714 + 2.35248 and 5.8188 ± 2.30181 for female and male, respectively [Table 6 and Figure 4]. Statistically no significant billirubin difference was observed between these two groups. P > 0.491
| Subjects | No. of subjects |
|---|---|
| Female | 6.2714 ± 2.35248 |
| Male | 5.8188 ± 2.30181 |
| t/p | –0.694/0.491 |
P is not significant
Table 6: Group statistics for TSB (mg/dl) levels between different sexes
Result from SPSS: From the data it is easy to interpret that, there is a significant difference found in S. Billirubin with age group 2 to 10 years and 21 to 30 years of age [Tables 7-10].
| Descriptives | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age Limit | N | Mean | Std. deviation | Std. error | 95% confidence interval for mean | Minimum | Maximum | ||
| Lower bound | Upper bound | ||||||||
| 2-10 yrs. | 18 | 4.7056 | 1.91694 | 0.45183 | 3.7523 | 5.6588 | 2.40 | 8.70 | |
| Billirubin | 11-20 yrs. | 16 | 5.8188 | 2.24773 | 0.56193 | 4.6210 | 7.0165 | 3.00 | 10.80 |
| 21-30 yrs. | 19 | 7.3737 | 2.01021 | 0.46117 | 6.4048 | 8.3426 | 3.20 | 10.80 | |
| Total | 53 | 5.9981 | 2.31022 | 0.31733 | 5.3613 | 6.6349 | 2.40 | 10.80 | |
Table 7: Table shows descriptive type of analysis of age on LFT
| ANOVA | ||||||
|---|---|---|---|---|---|---|
| Groups | Sum of squares | df | Mean square | F | Sig. | |
| Between Groups | 66.539 | 2 | 33.270 | 7.884 | 0.001 | |
| Billirubin | Within Groups | 210.991 | 50 | 4.220 | ||
| Total | 277.530 | 52 | ||||
Table 8: ANOVA table showing LFT on age group
| Dependent Variable | (I) age group | (J) age group | Mean difference (I-J) | Std. error | Sig. | 95% confidence interval | |
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| 2-10 yrs. | 11-20 yrs. | –1.11319 | 0.70581 | 0.363 | –2.8626 | 0.6352 | |
| 21-30 yrs. | –2.66813 | 0.67567 | 0.001 | –4.3419 | –0.9944 | ||
| Billirubin | 11-20 yrs. | 2-10 yrs. | 1.11319 | 0.70581 | 0.363 | –0.6352 | 2.8616 |
| 21-30 yrs. | –1.55493 | 0.69702 | 0.091 | –3.2816 | 0.1717 | ||
| 21-30 yrs. | 2-10 yrs. | 2.66813 | 0.67567 | 0.001 | 0.9944 | 4.3419 | |
| 11-20 yrs. | 1.55493 | 0.69702 | 0.091 | –0.1717 | 3.2816 | ||
Table 9: Table shows multiple comparisons (Bonferroni) on age group over LFT
| Independent sample test assumption= Equal variances assumed | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Levene’s test for equality of variances | t-test for equality of means | 95% confidence interval of the differences | |||||||
| F | Sig | t | df | Sig. (2 tailed) | Mean Differences | Std. Error Differences | Lower | Upper | |
| Billirubin | 0.069 | 0.794 | –0.694 | 51 | 0.491 | –0.45268 | 0.65205 | –1.76172 | 0.85637 |
Table 10: Table show Independent sample test (t-test) of LFT on different sex
Discussion
Thalassemia a group of genetic disorder occur mainly due to defective formation of globin chain of the hemoglobin moiety of the RBC. This specific type of blood disease results in excessive destruction of red blood cells which in turn leads to anemia. In this disease RBC breakdown occur at an early stage due to abnormal globin chain unable to protect RBC in oxidative stress. Resulting destruction of RBC leads to produce billirubin production which ultimately metabolized in liver for excretion. In thalassemia the rate of destruction of RBC is so rapid that it exceeds the liver capacity to metabolize the excess billirubin. [16-18] Hb E is the most common variant hemoglobin with a mutation in beta-globin gene causing substitution of glutamic acid for lysine at position 26 in beta-globin chain. Hb E Disease presents in 3 forms namely heterozygous state (Genotype AE or Hb E trait), homozygous state (Genotype EE or Hb E disease) and compound heterozygous states [1. Hb E beta-thalassemia (E-beta-thalassemia) 2. Sickle Cell/Hb E Disease (SE Genotype)]. [19-21]
Pathophysiology is complex which involves ineffective erythropoiesis, apoptosis, Oxidative damage and shortened red cell survival. Interaction between Hb E and betathalassemia alleles is main determinant in pathophysiology. Hb F level is strongest predictor of morbidity. Hb E Trait may be coinherited with either βo-thalassemia or β+-thalassemia. The compound heterozygous state is quite common in Thailand and occurs throughout a large part of Southeast Asia stretching from Indonesia to Sri Lanka, Northeast India and Bangladesh with prevalence rate of 30-40%, with very few. Pediatric cases being reported from India. [22-24]
In the study I enrolled LFT to observe the liver damage in thalassemic patient. I focus mainly the basic LFT such as S. Billirubin. S. billirubin is the first point that helps to recognized jaundice patient. I tried to find out the actual liver damage (hepatocellular/obstructive) in thalassaemic patient in different age group and different sex. My study is a prospective observational type of study done at Thalassaemia Sheba Kendra Chittagong with guidance from CMOSGH. In which study subjects are taken (Thalassemia patients) on different age and sex.
In accordance with other studies the most common recognized abnormality was excess billirubin turnover with excess RBC damage in relation to liver damage (change in ALT level with age). Three principal clinical pictures have been recognized: a. acute intrahepatic cholestasis, b. hepatic crisis and c. lithiasis . (Curcio et al., BMC Gastroenterology 2010, 10:117). Cholelithiasis and choledocholithiasis are common complications in patients with sickle cell disease or thalassemia. [25] The altered shape of red blood cells favors intravascular hemolysis and thus occlusion of the liver vascular bed, leading ultimately to tissue injury. Furthermore, hemolysis induces deposition of billirubin causing intrahepatic cholestasis and cholelithiasis. [26]
Conclusions
From the result of the study is that liver damage is augmented when age of the patients are increase. These are due to:
• increasing age with advancement of disease progression,
• repeated blood transfusion,
• Less use/intolerance of iron chelating agent,
• Decreased activity of hepatocyte to rescue them in such excess
billirubin and iron flood. Secondary to hyperspleenism.
From the overall study, we tried to correlate the liver damage in thalassemic patients with a hope to improve the liver damage in such patient with the goal of: (A) To prevent liver disease caused by viral hepatitis, iron overload, drug toxicity or hepatocellular carcinoma and (B) To monitor liver abnormalities routinely, and provide treatment for iron overload and any underlying liver disorder. The study revealed that in thalassemia patients when the age increases, the disease is progress with their complication. And in case of hepatic complication it is mainly due to hepatocellular in nature than that of obstructive one.
Acknowledgement
The authors thank Professor Dr. Mohammad Alauddin (Pro-vice Chancellor and founder chairman, Department of Biochemistry and Molecular Biology, University of Chittagong, Bangladesh) for encouragement and inspiration to complete the work. The authors especially thank Dr. Rana Chowdhury, Dr. Abdul Momen, Medical Officer, Department of Pediatric, Chattagram Maa-O-Shishu General Hospital, Chittagong and others colleagues for their kindness, outspoken behavior, valuable suggestions and encouragement throughout the research work.
References
- Khan WA. Thalassemia in Bangladesh. DS (Children) Hosp J 1999; 15:42-4.
- Modell B. Update to epidemiology of hemoglobin disorders with special references to thalassemia. Thalassemia International Federation. Internet. Transfus Med 1995;5:247-58.
- Khan WA. Prevention is the only way to combat Thalassemia. The Daily Star Web Edition 5, 1, Available from: http://www.rightdiagnosis. com/t/thalassemia/stats.htm [Last accessed on 2006 Feb 27.
- Weathall DJ, Clegg JB. Inherited Haemoglobin Disorders: An increasing global problem. Bull World Health Organ 2001;79:704-12.
- Shekhar HU, Kabir Y, Hossain MM, Mesbah-Uddin M, Khatun-EJannat K, Hossain MS, et al. Blood transfusion mediated viral infections in thalassemic children in Bangladesh. J Med Sci 2007;7:131-5.
- Weatherall DJ, Clegg JB. Thalassaemia- a global public health problem. Nat Med 1996;2:847-9.
- Wood WG, Weatherall DJ. Developmental genetics of the human hemoglobin’s. Biochem J 1983;215:1-10.
- Horkey A. Thalassemia-A project for a General Pathology college class. Available from: http://www.childrenscbf.org, http://blood.emedtv. com/thalassemia/causes-of-thalassemia.html, http://www.livestrong.com/article/197348-causes-of-thalassemia/, http://www.nlm.nih.gov/medlineplus/thalassemia.html, http://www.mayoclinic.com/health/thalassemia/DS00905, http://labtestsonline.org/understanding/conditions/thalassemia, http://www.rightdiagnosis.com/t/thalassemia/stats.htm, http:// www.freemd.com/alpha-thalassemia/incidence.htm. [Last accessed on 2012 Feb 10].
- Allen SJ, O’Donnell A, Alexander ND, Alpers MP, Peto TE, Clegg JB, et al. a+-thalassemia protects children against disease caused by other infections as well as malaria. Proc Natl Acad Sci USA 1997;94: 14736-41.
- Weatherall DJ. The thalassemia. In: Stamatoyannopoulos G, Nienhuis AW, Majerus PH, Varmus H, editors. The molecular basis of blood diseases. 2nd ed. Philadelphia: W.B. Saunders; 1994. p. 157-205.
- Weatherall DJ, Clegg JB. Thalassemia Syndrome, Tangvarasittichai Surapon, Chronic Diseases Research Unit, Department of Medical Technology, Naresuan University, Phitsanulok, Thailand. 2001;15: 329-68.
- Khan WA, Banu B, Amin SK. Prevalence of b- Thalassemia Trait and Hb E trait in bangladesh school children and health burden of thalassemia in our population. Dhaka Shishu (Child), Hosp J 2005;21:1-7.
- Giardina PJ, Forget BG, Hoffman R, Benz EJ, Shattil SS. Thalassemia syndromes. In: Hematology: Basic Principles and Practice. 5th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2008. p.46-9.
- Chernecky CC, Berger BJ. Laboratory tests and diagnostic procedures, 5th ed. St. Louis: Saunders; 2008. p.167-70.
- Aschaffenburg R, Mullen JE. A rapid and simple phosphatase test for milk. J Dairy Res 1949;16:58-67.
- Available from: http://medscape.com/article/958850-Overview.[Last accessed on 2008 Jan 08]. Available from: http://en.wikipedia.org/wiki/thalassemia.[Last accessed on 2008 July 18].
- Mohan H. Textbook of Pathology. 5th ed. New Delhi: Jaypee Brothers Publishers; 2006. p. 397-402.
- Lange PH, Millan JL, Stigbrand T, Vessella RL, Ruoslahti E, Fishman WH..Placental alkaline phosphatase as a tumor marker for seminoma. Cancer Res 1982;42:3244-7.
- Sarnaik AS. Thalassemia and related haemoglobinopathies. (ALP: The Test) Indian J Pediatr 2005;72:319-24.
- Lange PH, Millan JL, Stigbrand T, Vessella RL, Ruoslahti E, Fishman WH. Placental alkaline phosphatase as a tumor marker for seminoma. Cancer Res 1982;42:3244-7.
- Schiele F, Vincent-Viry M, Fournier B, Starck M, Siest G. Biological effects of eleven combined oral contraceptives on serum triglycerides, gamma glutamyltransferase, alkaline phosphatase, billirubin and other biochemical variables. Clin Chem Lab Med 1998;36:871-8.
- Hann IM, Smith OP. Pediatric hematology. USA: Wiley-Blackwell; 2006. p. 763.
- Berk PD, Korenblat KM. Approach to the patient with jaundice or abnormal liver test results. In: Goldman L, Ausiello D, editors. Cecil Medicine. 23rd edn. Philadelphia, PA: Saunders Elsevier; 2007.
- Pirone C, Quirke JM, Priestap HA, Lee DW. The animal pigment billirubin discovered in plants. J Am Chem Soc 2009;131:2830-9.
- McDonagh AF, Palma LA, Palma LA, Lightner DA. Blue light and billirubin excretion. Science 2002;208:145-51.