A new venture with sclerotherapy in an oral vascular lesion
- *Corresponding Author:
- Dr. G. Sitra
Department of Oral Medicine and Radiology, Indira Gandhi Institute of Dental Sciences, Sri Balaji Vidyapeeth University, Puducherry - 607 402, India.
E-mail: sitrag@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Vascular malformations are one of the most common lesions of the oral cavity. The lesion may be a congenital malformation observed in neonates or arteriovenous malformation observed in adults. Various surgical and medical managements are possible for vascular lesions which include surgical excision, laser therapy, cryotherapy, selective embolization, intralesional sclerosing agents, β‑blockers and steroid therapy. Here we report a case of oral vascular lesion where intralesional injection with 30 mg/ml of sodium tetradecyl sulfate (STS) was given, which resulted in local complications with severe inflammatory response including pain, swelling, and surface ulceration that remained for 2 weeks. Sclerotherapy with STS still remain an effective agent in treating benign oral vascular lesions and provides alternative or support for surgical methods. Sometimes it can lead to undesirable complications like allergic reactions, local inflammatory response, etc.
Keywords
Arteriovenous malformation, sclerotherapy, sodium tetradecyl sulfate
Introduction
Vascular malformations (VM) are a general term used to describe a group of lesions formed by an anomaly of the capillary, venous, lymphatic, and arterial system. These are structural anomalies of blood vessels without endothelial proliferation which presents at birth, commonly manifest in childhood or adolescence and persist throughout life. [1] They can be categorized according to the type of vessels involved (capillary, venous, arterial) and according to hemodynamic features (low flow or high flow). [2] They can be treated with sclerosing agent with better patient compliance. This paper highlights a case of an intraoral vascular malformation treated with intralesional sclerosing agent which resulted in severe local inflammatory response and its management in the dental office.
Case Report
A 55-year-old male patient presented with a swelling involving the right half of the tongue since childhood, which gradually increased in size for the past 20 years. There was no history of pain, ulceration, difficulty in speech and swallowing. The past medical, dental, and family history was noncontributory.
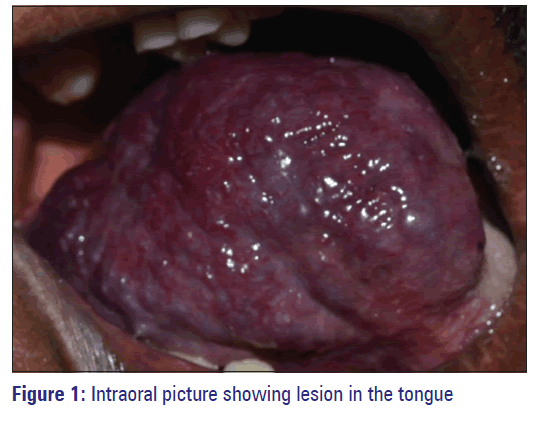
On intraoral examination, a localized dome-shaped swelling measuring approximately 6 cm × 7 cm was present in the right dorsum and lateral aspect of the tongue. Borders of the swelling were well defined, and it extended anteroposteriorly from the tip of the tongue to the posterior one third of tongue, mediolaterally from the middle of the tongue to the lateral border of the tongue. It was pinkish red in color with irregular pebbled surface, and the surrounding area appeared pale pink in color [Figure 1]. There was no visible pulsation. On palpation, it was soft to firm in consistency, immobile, and nontender. There was no palpable thrill, but the swelling blanched on compression with a glass slide (diascopy) [Figure 2].
Based on the history and clinical features, a working diagnosis of arteriovenous malformation (AVM) with differential diagnosis of hemangioma and lymphangioma was arrived following which necessary radiologic investigations were carried out.
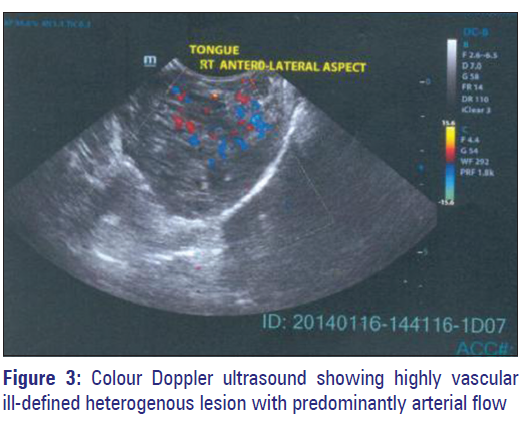
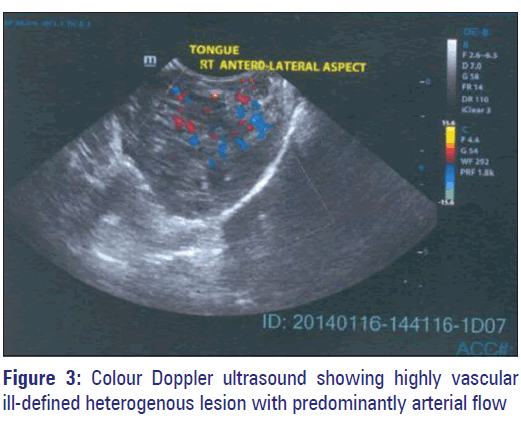
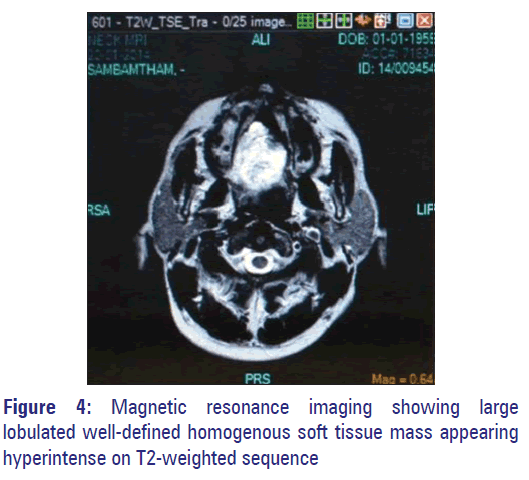
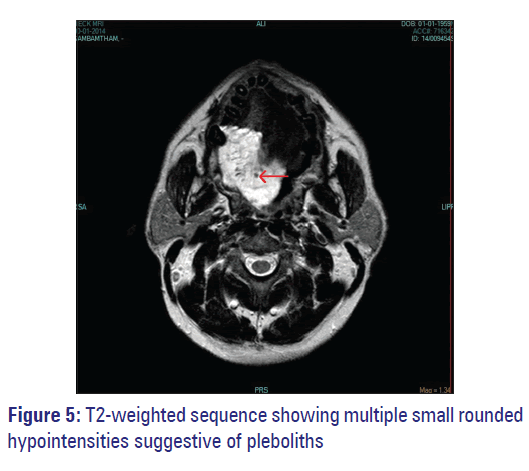
Color Doppler ultrasound (US) revealed an ill-defined heterogenous lesion in the right anterior, lateral, and posterior aspect of the tongue. The lesion was highly vascular with no feeder vessel. Flow inside the lesion was predominantly arterial [Figure 3]. Magnetic resonance imaging (MRI) revealed a large lobulated well-defined homogenous soft tissue mass in the right half of the tongue measuring 40 mm × 46 mm × 60 mm which appeared hyperintense on T2-weighted sequence [Figure 4] with multiple phleboliths [Figure 5].
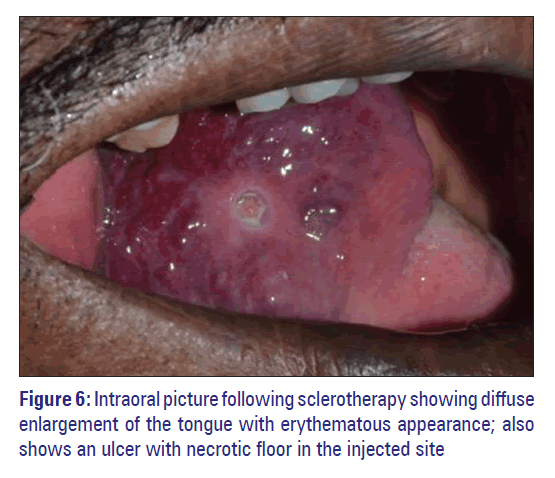
Considering the provisional diagnosis, unwillingness of the patient for surgery, management with intralesional injection of 30 mg/ml of sodium tetradecyl sulfate (STS) was decided with the consent of the patient. In the first visit after anesthetizing the area, intralesional injection with 1 ml of 3% STS diluted with 4 ml of distilled water was given using a 25 gauge needle at multiple sites. The next day the patient presented with painful diffuse enlargement of the tongue which appeared erythematous with multiple ulcers with tender necrotic floor in the injected sites [Figure 6]. He did not report any systemic symptoms and his vital signs were normal. It was clinically diagnosed as severe local inflammatory reaction to the sclerosing agent and was managed immediately with intramuscular injections of dexamethasone (2 mg) and chlorphenaramine maleate (25 mg) followed by oral intake of chlorphenaramine maleate tablet (25 mg) for 3 days. Patient was recalled for the next 3 days for review and irrigation of the ulcer was done with hydrogen peroxide. Patient was recalled after a week to ensure complete resolution of local inflammatory response and healing of ulcers in the injection site.
Discussion
The International Society for the Study of Vascular Anomalies Classification divides vascular anomalies into two primary biological categories: (1) Vasoproliferative or vascular neoplasms and (2) VM. [3] VM occur in approximately 1% of births but majority of these patients do not present for treatment. These lesions can occur at any area of the body; gradual in onset and progression. The most common sites in the oral cavity are anterior two-thirds of the tongue, palate, and gingiva and buccal mucosa. [1] In our case, the lesion was present in the tongue since childhood, and it was gradually increasing in size which can be correlated with the features of AVM.
Vascular malformations in the oral cavity cause discomfort and potentially serious clinical problems. Tongue lesions can cause problems such as recurrent hemorrhage, biting of the lesion, pain, and difficulty with speaking, mastication or deglutition. [4] Our patient gave a history of difficulty in swallowing and occasional biting of the lesion.
Color Doppler US of AVM shows arterial and venous signals from vessels in the lesion and often appears hypervascular. MRI is helpful to further characterize sonographic findings and determine the extent of larger lesions for planning medical, interventional, and/or surgical therapy. [5] The present case appeared highly vascular with no feeder vessel in doppler US and hyperintense on MRI T2-weighted sequence with multiple phleboliths.
Treatment of benign vascular lesions includes surgery, systemic corticosteroids, interferon-α, laser, embolization, sclerotherapy, cryotherapy, and radiation. [6] The treatment employed in the present case was sclerotherapy which is the best complement to subsequent surgery.
Advantages of sclerosing agent are that it is simple, inexpensive, readily available, hospitalization not required and cause no blood loss. Disadvantages are postoperative pain and burning sensation, anaphylactic reaction, tissue necrosis, and sloughing (4%) and airway compromise (1%). [7]
Sodium tetradecyl sulfate has been used for many decades as a sclerosant with a high level of safety and efficacy. Chemically, this drug is unique unto itself and unrelated to other commonly used sulfur-containing pharmacologics that normally have a strong allergic potential. [8] It works by causing localized inflammatory reaction, obliterative thrombosis of hemangiomatous space, subsequent fibrosis of the endothelial spaces, regression of the lesion without affecting the bone. [9]
There have been reports of anaphylactic reaction and pulmonary embolism following intravenous injection of STS. [8] Minkow et al., in their study using intralesional injection of 3% (STS) in intraoral hemangioma showed satisfactory results in all patients with minimum side effects [10] whereas in another study on venous malformations using 3% STS, complications occurred [11] similar to our case.
Conclusion
The management of vascular lesions is challenging. Though sclerotherapy produces local complications as we encountered in our case, it proves to be an effective; conservative technique for the same and the dentist treating with sclerosants also should be prepared to deal with this type of situations.
References
- Manjunath SM, Shetty S, Moon NJ, Sharma B, Metta KK, Gupta N, et al. Arteriovenous malformation of the oral cavity. Case Rep Dent 2014;2014:353580.
- Monteiro LS, Azevedo A, Cadilhe S, Sousa D, Faria C, Martins M. Laser treatment of vascular anomalies of oral cavity. Rev Port Stomatol Med Dent Maxillofac Surg 2013;54:171-5
- Kamala KA, Ashok L, Sujatha GP. Cavernous hemangioma of the tongue: A rare case report. Contemp Clin Dent 2014;5:95-8.
- Shetty DC, Urs AB, Rai HC, Ahuja N, Manchanda A. Case series on vascular malformation and their review with regard to terminology and categorization. Contemp Clin Dent 2010;1:259-62.
- Duncan C, Fourie PA. Vascular malformations. Part 2. Current classification of vascular malformations. S Afr J Radiol 2004;8:23-30.
- Mulliken JB, Fishman SJ, Burrows PE. Vascular anomalies. Curr Probl Surg 2000;37:517-84.
- Parvathidevi MK, Koppal S, Rukmangada T, Byatnal AR. Management of haemangioma with sclerosing agent: A case report. BMJ Case Rep 2013;2013.
- Crippen C. Anaplylactic reaction to sodium tetradecyl sulphate after sclerotherapy: A case report. Phlebologie 2011;64:47-8.
- Marler JJ, Mulliken JB. Current management of hemangiomas and vascular malformations. Clin Plast Surg 2005;32:99-116, i ×.
- Minkow B, Laufer D, Gutman D. Treatment of oral hemangiomas with local sclerosing agents. Int J Oral Surg 1979;8:18-21.
- Bajpai H, Bajpai S. Comparative analysis of intralesional sclerotherapy with sodium tetradecyl sulfate versus bleomycin in the management of low flow craniofacial soft tissue vascular lesions. J Maxillofac Orala Surg 2012;11:13-20.